Int J Pediatr Otorhinolaryngol:耳蜗植入对不对称感觉神经性听力损失儿童言语和语言的影响
2021-12-15 AlexYang MedSci原创
调查了单侧CI对ASHL儿童患者的言语和语言结果的影响。
对于非对称性感觉神经性听力损失(ASHL)或单耳重度至深度感觉神经性听力损失,且对侧听力较好的儿童,可考虑进行人工耳蜗植入(CI)。在上述这些儿童中,CI的益处还没有很好地阐释。
近期,来自美国的研究人员在《Int J Pediatr Otorhinolaryngol》杂志上发表文章,调查了单侧CI对ASHL儿童患者的言语和语言结果的影响。
研究鉴定了2014年至2017年间,在一家三级单中心机构接受人工耳蜗植入治疗的儿童患者。纳入了在听力较差耳朵接受人工耳蜗植入,并在听力较好耳朵使用助听器的儿童,排除了有认知障碍或先前有耳蜗神经缺损和听觉神经病变的儿童。研究人员在植入前和植入后每隔6个月定期评估言语和语言结果。每次就诊时,都会对耳部特异性测听进行评估。研究人员还对言语清晰度、表达和接受语言以及词汇进行了评估,包括Goldman Fristoe发音测试(GFTA-3)、语言基础临床评估(CELF-P2或CELF-5)、接受性单字图片词汇测试(ROWPVT)和表达性单字图片词汇测试(EOWPVT)。计算了术前和术后言语和语言结果的平均差异和标准偏差,并进一步评估了术后各时间点的结果变化。
共有26名患有非对称性感觉神经性听力损失的儿童纳入了分析,其中11名(42%)有双侧前庭导水管扩大(EVA)。在进行CI时,较好耳朵的无辅助纯音平均值(PTA-4)为62Db HL,较差耳朵为92Db HL。耳蜗植入的耳朵在语言识别方面存在改善。有23名患者在术后至少进行了一次重新评估。14名患者使用了相同的工具进行了术前和术后评估,其中13名患者(93%)至少在一个领域中改善。在术后12个月进行重复评估的患者中,他们的GFTA-3(+11.2)、CELF-P2核心语言(+10.3)、CELF-5核心语言(+7.0)、ROWPVT(+2.8)和EOWPVT(+4.5)均有改善。
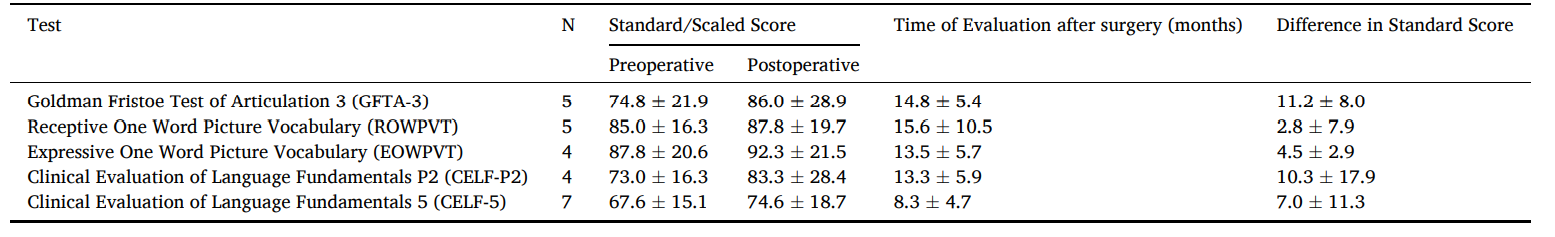
耳蜗植入后言语和语言测试结果情况
综上所述,在接受单侧人工耳蜗植入治疗的非对称性感觉神经性听力损失儿童中,其言语和语言方面具有改善。虽然这些儿童并不是典型的CI候选人,但他们可以从较差耳朵的CI中受益。
原始出处:
Prashant S Malhotra , Jaron Densky , Manasa Melachuri et al. The impact of cochlear implantation on speech and language outcomes in children with asymmetric sensorineural hearing loss. Int J Pediatr Otorhinolaryngol. Nov 2021
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#DIA#
49
#PE#
40
#感觉神经#
45
#神经性#
56
#听力#
52
#语言#
40
#植入#
29
#耳蜗植入#
33
于广泛期SCLC患者,铂类为基础的化疗是
54