Cell Death & Disease:能帮助抑制慢性肾脏疾病的酶
2021-07-18 Viho MedSci原创
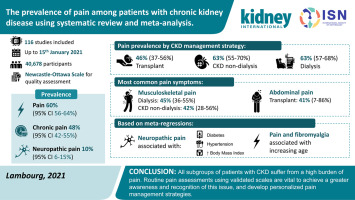
慢性肾脏病(CKD)是指随着时间推移,肾脏功能的下降而导致的,这种疾病影响着全球近10%的人口。
慢性肾脏病(CKD)是指随着时间推移,肾脏功能的下降而导致的,这种疾病影响着全球近10%的人口。越来越多的证据表明,过量的钠+消费可以加速CKD的进展,并通过多种机制导致终末期肾病(Esrd),包括高血压引起的动脉血压升高。
南澳大利亚大学的研究人员已经确定了一种可能有助于抑制CKD的酶,这种名为NEDD4-2的酶对肾脏健康至关重要,这项研究发表在 Cell Death & Disease杂志上。
高盐饮食会加重某些类型的肾脏疾病,直到现在,研究人员还没有意识到NEDD4-2在盐引起的肾脏损害中起着促进作用。科学家们在一项动物研究中展示了高盐饮食、低水平NEDD4-2水平与晚期肾病之间的相关性。

高钠加重肾脏疾病和NEDD4-2含量低
研究表明高钠饮食和低NEDD4-2水平都会促进肾脏疾病的发展,即使在没有高血压的情况下,高血压通常与钠含量增加同时发生。NEDD4-2调节钠在肾脏中重新吸收所需的途径,以确保保持正确的盐水平。如果NEDD4-2蛋白减少或被抑制,盐吸收增加会导致肾脏损害。
即使是低盐饮食的人,如果他们有低水平的NEDD4-2水平,由于基因的变异或突变,他们也会受到肾脏损害。
糖尿病肾病--肾脏疾病的一个常见原因--NEDD 4-2水平严重下降。即使盐不是一个因素,情况也是如此。这项研究还揭示了一个令人惊讶的发现:高盐饮食引起的肾脏疾病并不总是由高血压引起的。在很多情况下,高血压会加重肾脏疾病,高盐饮食会导致过多的失水和低血压,这意味着没有高血压的人也会患上肾病。
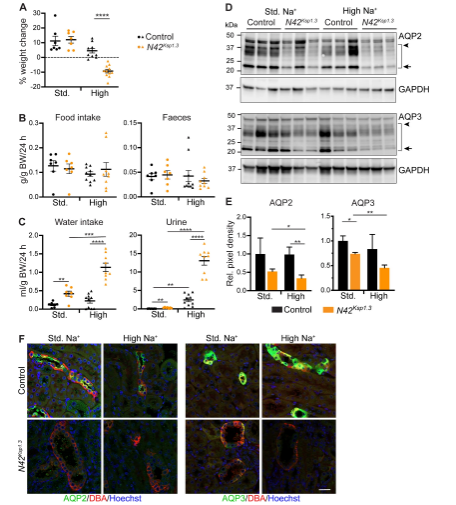
体重减轻、多尿、电解质失衡与肾脏疾病
“柳叶刀”2020年的一篇论文估计,约7亿人--即世界人口的10%--患有慢性肾脏疾病,在过去30年里增加了29%。CKD的激增主要归因于近几十年来全球肥胖的流行,糖尿病是导致慢性肾脏疾病和高血压的主要原因之一。世界卫生组织(World Health Organization)的统计数据显示,1980年至2014年间,糖尿病发病率增长了300%,成为全球十大死因之一,科学家们试图解决肾脏疾病所面临的问题的严重性。
肥胖和生活方式是导致慢性肾脏疾病的两个主要因素,但也有其他因素在起作用。急性肾损伤、因其他原因服用的药物、高血压和遗传易感性也可能导致这一疾病。
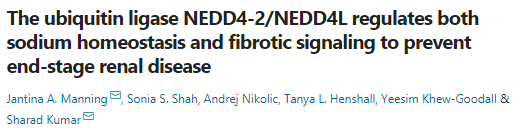
文章参考:Jantina A. Manning, Sonia S. Shah, Andrej Nikolic, Tanya L. Henshall, Yeesim Khew-Goodall, Sharad Kumar. The ubiquitin ligase NEDD4-2/NEDD4L regulates both sodium homeostasis and fibrotic signaling to prevent end-stage renal disease. Cell Death & Disease, 2021; 12 (4) DOI: 10.1038/s41419-021-03688-7
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#Dis#
61
#Cell#
48
#CEL#
45
#Death#
48
#慢性肾脏#
33
签到
46
非要有意义
63