NEJM:瑞博西尼加来曲唑治疗晚期乳腺癌的总体生存率
2022-03-10 MedSci原创 MedSci原创
在HR阳性、HER2阴性晚期乳腺癌患者中,与安慰剂加来曲唑相比,瑞博西尼加来曲唑的一线治疗能具有显著的总体生存获益。瑞博西尼的中位总生存期比安慰剂长12个月以上。
激素受体(HR)阳性、人表皮生长因子受体2(HER2)阴性疾病是转移性乳腺癌最常见的亚型,并且仍然无法治愈。在之前对该3期试验的分析中,在激素受体(HR)阳性、人表皮生长因子受体2(HER2)阴性的绝经后患者中,与单独采用来曲唑治疗相比,晚期乳腺癌采用一线瑞博西尼加来曲唑治疗的无进展生存期显著延长。不知道瑞博西尼的总生存期是否也会更长。

近日,顶级医学期刊NEJM上发表了一篇研究文章,研究人员报告了方案指定的总生存期最终分析结果,这是一个关键的次要终点。患者以1:1的比例随机分配接受瑞博西尼或安慰剂联合来曲唑。
此外,研究人员使用分层对数秩检验评估总生存率,并在发生400例死亡后使用Kaplan-Meier方法进行总结,并采用分层测试策略分析无进展生存期和总生存期,以确保研究结果的有效性。
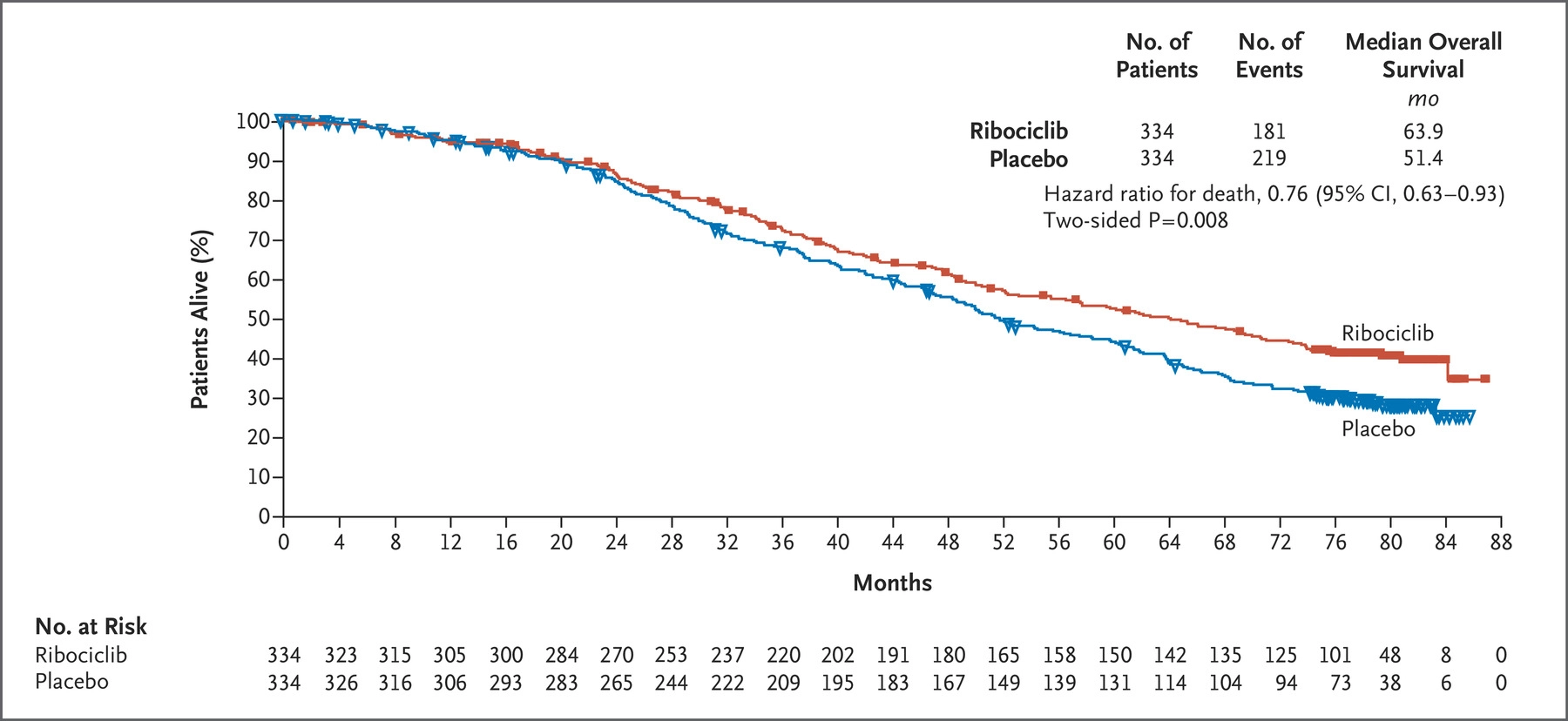
中位随访6.6年后,瑞博西尼组334名患者(54.2%)发生181例死亡病例,安慰剂组334例(65.6%)患者发生219例死亡病例。与安慰剂加来曲唑相比,瑞博西尼加来曲唑具有显著的总体生存获益。瑞博西尼加来曲唑的中位总生存期为63.9个月(95%CI为52.4至71.0),安慰剂加来曲唑为51.4个月(95%CI为47.2至59.7)(死亡风险比为0.76;95%CI为0.63至0.93;两侧P=0.008)。没有观察到新的安全性事件。
由此可见,在HR阳性、HER2阴性晚期乳腺癌患者中,与安慰剂加来曲唑相比,瑞博西尼加来曲唑的一线治疗能具有显著的总体生存获益。瑞博西尼的中位总生存期比安慰剂长12个月以上。
原始出处:
Gabriel N. Hortobagyi,et al.Overall Survival with Ribociclib plus Letrozole in Advanced Breast Cancer.NEJM.2022.https://www.nejm.org/doi/full/10.1056/NEJMoa2114663
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#总体生存率#
43
#生存率#
44
#来曲唑#
62
学习
61