JAMA Oncol:对于激素受体阳性乳腺癌,帕博西尼 ➕来曲唑 优于帕博西尼 ➕氟维司群
2021-10-19 MedSci原创 MedSci原创
在内分泌敏感、激素受体阳性、ERBB2阴性晚期乳腺癌患者中,来曲唑是帕博西尼的首选合作伙伴。
乳腺癌是女性的头号杀手。在2020年,全球新增 226 万 万乳腺癌症患者。乳腺癌的新增人数已经超过了肺癌,成为全球第一大癌症。
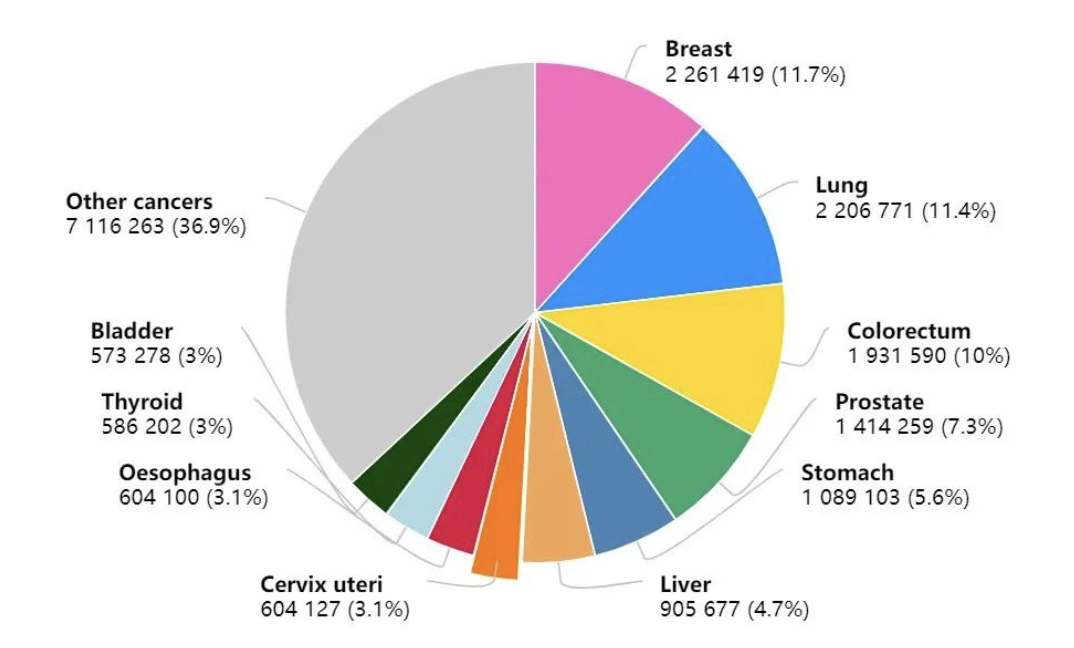 2020年癌症新发病例数前十的癌症类型
2020年癌症新发病例数前十的癌症类型
随着医学的进步,激素受体阳性乳腺癌的药物也越来越多。比如Palbociclib(帕博西尼)、来曲唑和氟维司群。
Palbociclib(帕博西尼)是全球首个批准上市的CDK4/6激酶抑制剂,是一种实验性、口服、靶向性CDK4/6抑制剂,可阻断肿瘤细胞的增殖,是治疗晚期乳腺癌的一种药物。作为口服治疗药物,医学界认为CD4/6靶点药物帕博西尼和HER2靶点药物曲妥珠单抗(赫赛汀)是如今针对性治疗乳腺癌比较好的靶向药物。

帕博西尼在国内上市后,改成爱博新。

在临床中,帕博西尼和来曲唑、氟维司群的联合治疗都优于来曲唑或氟维司群的单独治疗效果。 但是对于先前未经治疗的内分泌敏感、激素受体阳性、ERBB2阴性晚期乳腺癌中,帕博西尼的最佳内分泌搭档是氟维司群还是来曲唑呢?
近期一项发表在JAMA oncology 上的一项研究表明,氟维司群- 帕博西尼与来曲唑- 帕博西尼 相比在无进展生存期方面没有改善,证实来曲唑是该患者群体中首选的帕博西尼合作伙伴。
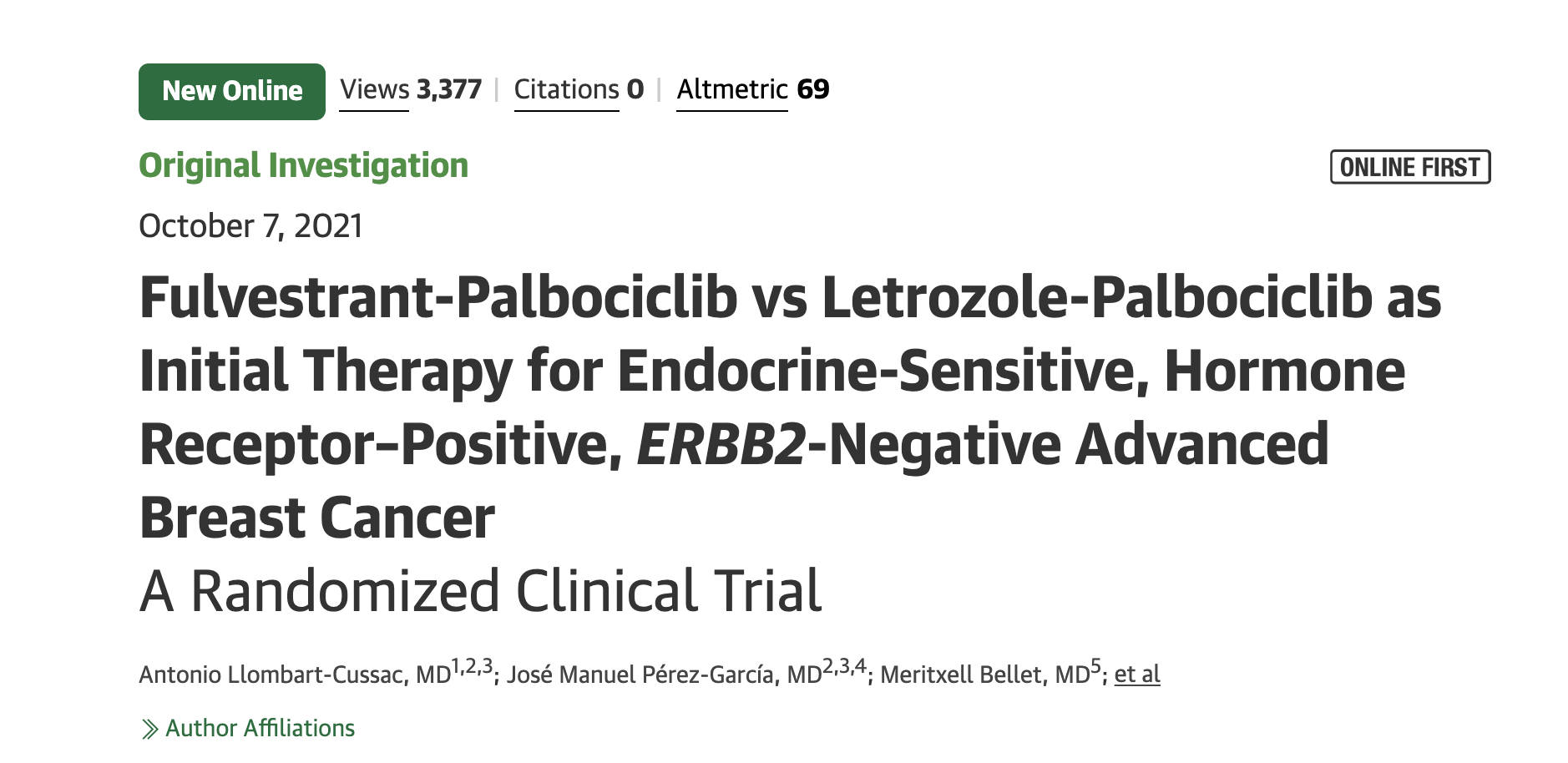
在这项于2015年7月30日-2018年1月8日期间进行的国际、随机、开放标签、2 期临床研究中,受试者为激素受体阳性、ERBB2阴性、既往未接受过治疗的晚期乳腺癌患者。
患者被随机分配(1:1 比例)接受 帕博西尼 和氟维司群或来曲唑。分层因素是疾病表现的类型(新发与复发)和内脏受累的存在(是与否)。主要终点是研究者评估的无进展生存期,该无进展生存期由实体瘤反应评估标准 1.1 版确定。
研究结果发现,氟维司群-帕博西尼组的中位研究者评估无进展生存期为 27.9 个月(95% CI,24.2-33.1 个月),而来曲唑-帕博西尼组为 32.8 个月(95% CI,25.8-35.9 个月)(风险比, 1.13;95% CI,0.89-1.45;P = .32)。差异无统计学意义。这一结果在所有分层因素中都是一致的。
此外,氟维司群-帕博西尼和来曲唑帕博西尼的客观缓解率(46.5% 对 50.2%)和3年总生存率(79.4% 对 77.1%)未观察到显着差异。3-4 级不良事件在治疗组之间具有可比性,并且没有发现新的安全性信号。没有报告与治疗相关的死亡。
尽管氟维司群-palbociclib 显示出显著的抗肿瘤活性,但这项随机临床试验未能确定在内分泌敏感、激素受体阳性、ERBB2阴性晚期乳腺癌患者中,该方案与来曲唑-palbociclib 相比可改善无进展生存期癌症。因此,来曲唑是该患者群体中首选的帕博西尼合作伙伴。
参考文献:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言















#激素受体阳性#
43
#Oncol#
45
#来曲唑#
61
#帕博西尼#
52
其中的机制有研究文献吗
85