Eur Urol:前列腺特异性膜抗原放射引导手术检测前列腺癌患者的淋巴结转移
2022-08-25 AlexYang MedSci原创
描述了RARP期间,PSMA-RGS的2期前瞻性研究(NCT04832958)的中期分析结果。
扩展盆腔结节清扫术(ePLND)是前列腺癌(PCa)结节分期的金标准。前列腺特异性膜抗原(PSMA)放射引导手术(RGS)可以在机器人辅助前列腺根治术(RARP)中识别淋巴结侵犯(LNI)。

近期,来自意大利的研究人员在《Eur Urol》上发表文章,描述了RARP期间,PSMA-RGS的2期前瞻性研究(NCT04832958)的中期分析结果。
研究为一项2期试验,旨在招募100名常规影像学检查中诊断为中危或高危cN0cM0 PCa的患者,其LNI风险>5%。总体而言,2021年6月-2022年3月期间,有18名患者入组。其中,12名患者接受了PSMA-RGS,代表研究队列。
所有患者都接受了68Ga-PSMA正电子发射断层扫描(PET)/磁共振成像;99mTc-PSMA-I&S在手术前一天合成并静脉注射,然后进行单光子发射计算机断层扫描/计算机断层扫描。Drop-In伽马探针用于体内测量。所有阳性病变(与背景相比计数率≥2)均切除,并行ePLND。结果为评估了机器人辅助PSMA-RGS治疗LNI的副作用、围手术期结果和性能特点。
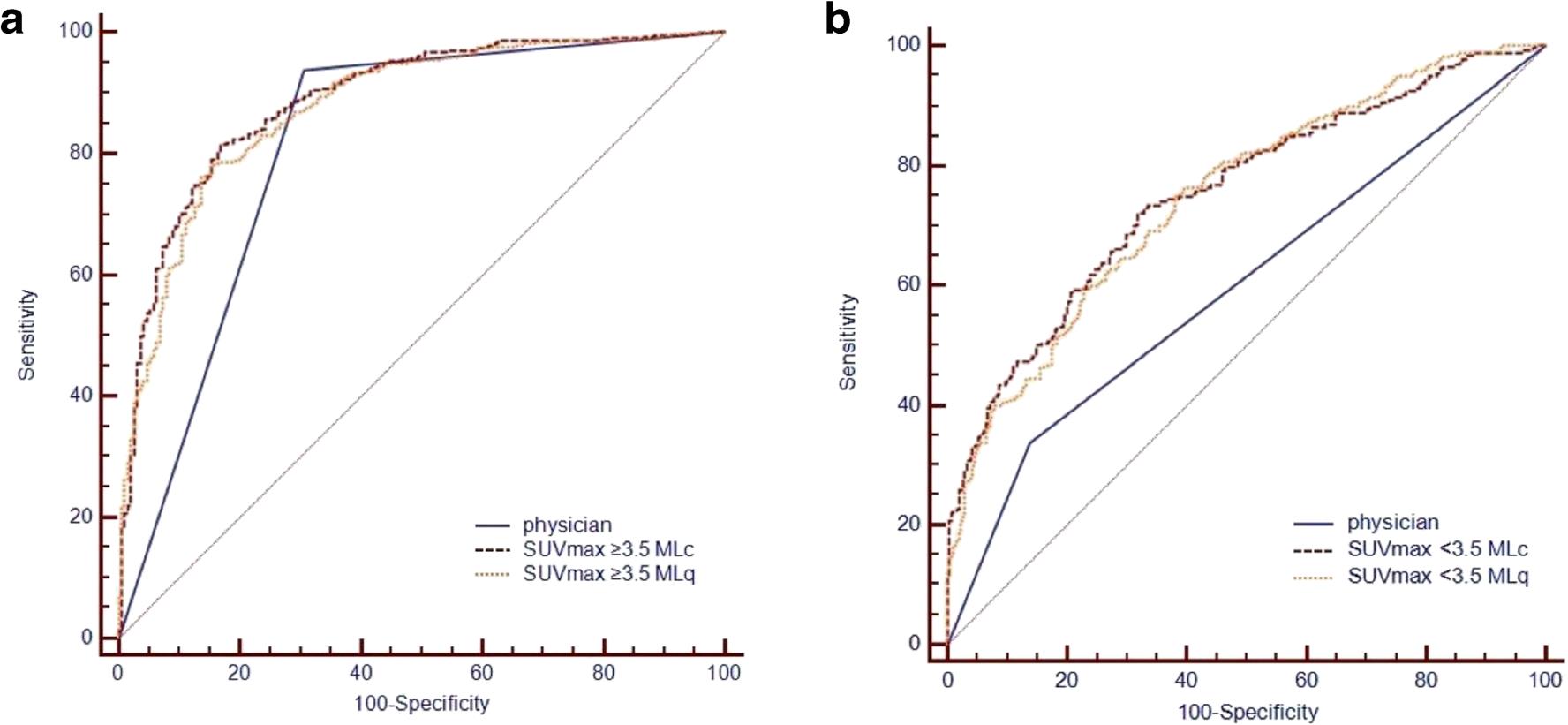
研究中有4名(33%)、6名(50%)和2名(17%)患者分别为中危、高危和局部晚期PCa。2名(17%)患者在PSMA PET时有病理结点摄取。手术时间、失血量和住院时间的中位数分别为230分钟、100毫升和5天。没有不良事件和术中并发症的记录。1名患者出现了30天的并发症(Clavien-Dindo 2;8.3%)。3名(25%)患者在ePLND时存在LNI。在对96个结节区域进行逐一分析时,PSMA-RGS的敏感性、特异性、阳性预测值和阴性预测值分别为63%、99%、83%和96%。在每个病人层面上,PSMA-RGS的敏感性、特异性、阳性预测值和阴性预测值分别为67%、100%、100%和90%。
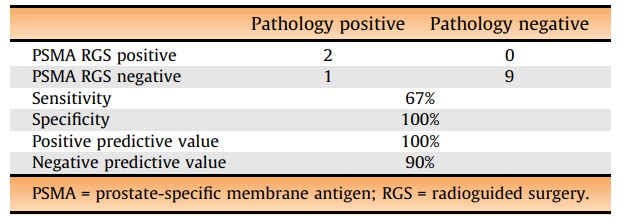
单个患者的诊断准确性情况
综上所述,机器人辅助PSMA-RGS在初级分期中是一种安全和可行的方法,特异性良好,但敏感性欠佳,可能会遗漏微转移性结节疾病。
原始出处:
Giorgio Gandaglia , Elio Mazzone , Armando Stabile et al. Prostate-specific membrane antigen Radioguided Surgery to Detect Nodal Metastases in Primary Prostate Cancer Patients Undergoing Robot-assisted Radical Prostatectomy and Extended Pelvic Lymph Node Dissection: Results of a Planned Interim Analysis of a Prospective Phase 2 Study. Eur Urol. Jul 2022
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#特异性#
67
#前列腺特异性膜抗原#
42
#淋巴结#
65
#淋巴结转移#
53
#抗原#
53