JAHA:静脉血栓栓塞后肺动脉高压的发生率和危险因素
2022-07-17 MedSci原创 MedSci原创
在这一项大型的真实世界的VTE人群中,3.5%的患者在最初的VTE事件发生后的2年内发生PH。随着年龄的增长,在发生静脉血栓栓塞事件时有其他合并症的女性中,风险较高。
肺动脉高压(PH)是肺栓塞一种致命性的潜在并发症,表现为静脉血栓栓塞(VTE)。既往有静脉血栓栓塞者PH的发生率和危险因素尚未明确。

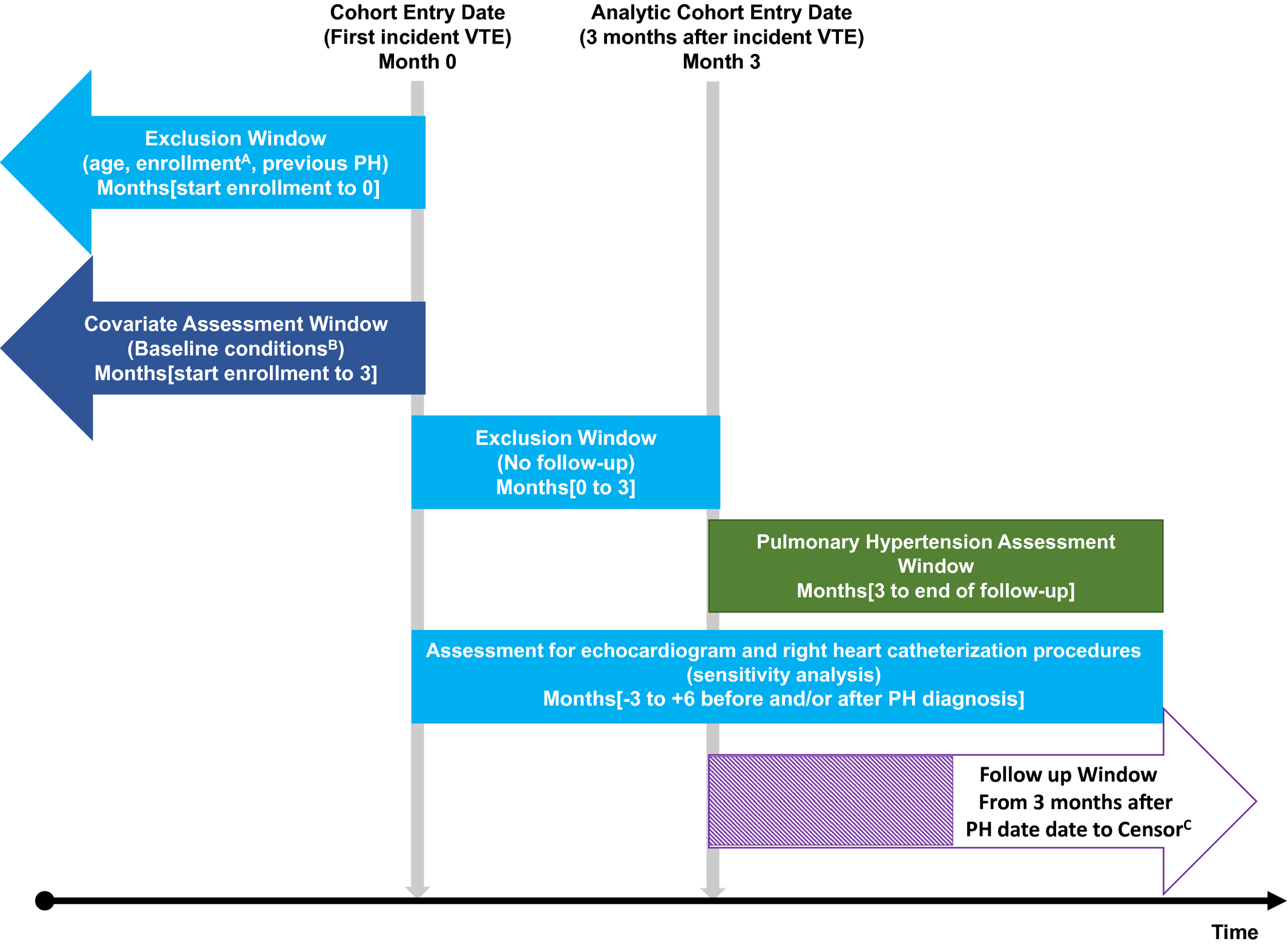
近日,心血管疾病领域权威杂志JAHA上发表了一篇研究文章,研究人员采用来自MarketScan管理数据库2011-2018年期间住院和门诊医疗索赔的国际疾病分类(ICD)代码识别静脉血栓栓塞的病例、静脉血栓栓塞事件前的合并症以及静脉血栓栓塞事件后发生的PH。研究人员计算了累积发生率和风险比(HR)及其95%CI。
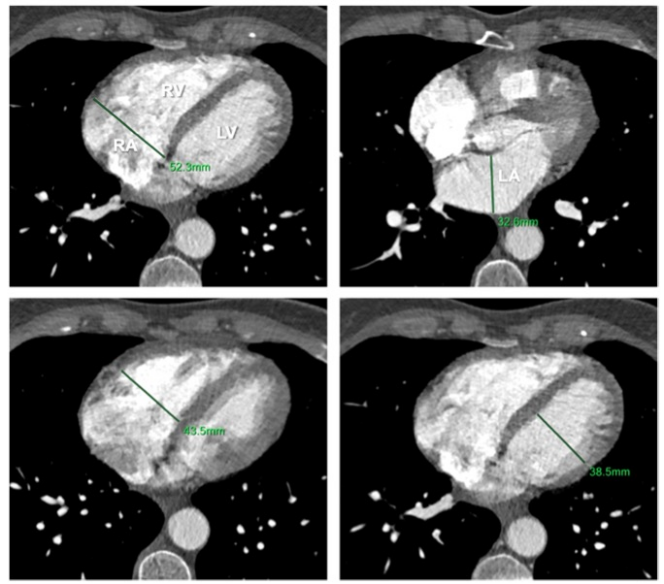
纳入分析的170021例VTE患者平均(±SD)年龄为57.5±15.8岁,其中50.5%为女性。在平均1.94年的随访期间,累计共有5943例PH病例。发生VTE后2年,PH的累积总体发生率(95%CI)为3.5%(3.4%-3.7%)。老年患者(3.9%[3.8%-4.1%])高于男性(3.2%[3.0%-3.3%]),肺栓塞(6.2%[6.0%-6.5%])高于仅存在深静脉血栓的患者(1.1%[1.0%-1.2%])。调整年龄和性别后,伴有潜在合并症的静脉血栓栓塞患者发生PH的风险更高。使用Charlson合并症指数可观察到剂量-反应关系,评分越高,PH风险越高(评分≥5 vs. 0:HR(2.50[2.30-2.71]))。在评估单一合并症时,其与心衰(HR为2.17[2.04-2.31])、慢性肺部疾病(HR为2.01[1.90-2.14])和酗酒(HR为1.66[1.29-2.13])的相关性最强。
由此可见,在这一项大型的真实世界的VTE人群中,3.5%的患者在最初的VTE事件发生后的2年内发生PH。随着年龄的增长,在发生静脉血栓栓塞事件时有其他合并症的女性中,风险较高。这些数据为了解静脉血栓栓塞患者的PH负担和PH的危险因素提供了深入的见解。
原始出处:
Pamela L. Lutsey.et al.Incidence and Risk Factors of Pulmonary Hypertension After Venous Thromboembolism: An Analysis of a Large Health Care Database.JAHA.2022.https://www.ahajournals.org/doi/10.1161/JAHA.121.024358
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#动脉高压#
44
#静脉血#
59
#静脉#
0
#发生率#
41
#AHA#
47