Eur Heart J:左心疾病引起肺动脉高压患者肺血管疾病的病理生理学意义
2022-07-12 MedSci原创 MedSci原创
LHD中的肺血管疾病与病理生理特征相关,其特征为运动引起的肺充血、动脉低氧血症、RV-PA解耦、心室相互依赖以及氧输送受损、有氧能力受损。需要进一步的研究来确定新的治疗PH-LHD的方法。
肺动脉高压(PH)和肺血管疾病(PVD)是常见的,并与左心疾病(LHD)的不良结局相关。近日,心血管领域权威杂志Eur Heart J上发表了一篇研究文章,该研究试图通过LHD的PH谱来归纳总结PVD的病理生理特征。

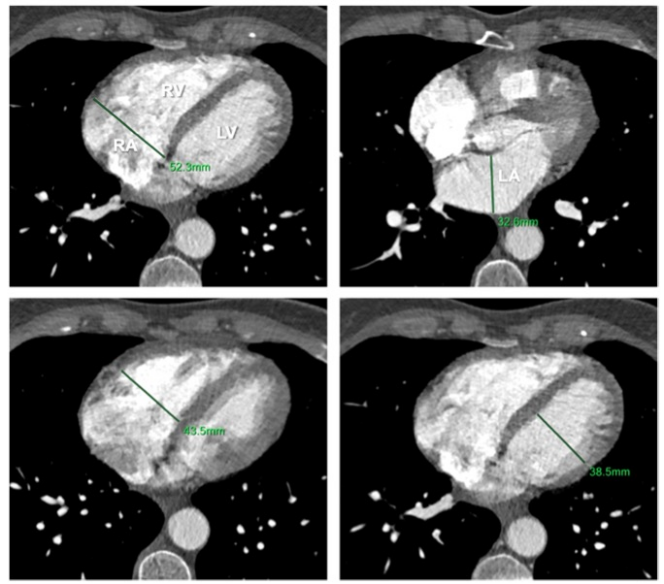
在这项前瞻性研究中,PH-LHD(平均肺动脉压(PA)>20mmHg,肺动脉楔压(PAWP)≥15mmHg)患者和无PH或LHD的对照组同时进行有创血流动力学运动检测,同时进行超声心动图、呼气和血气分析和肺超声检查。根据肺血管阻力(PVR<3.0或≥3.0WU)将PH-lhd患者分为单纯的毛细血管后PH(IpcPH)和联合的毛细血管后及前PH(CpcPH)。
与对照组(n=69)和IpcPH-LHD(n=55)相比,CpcPH-LHD(n=40)患者在休息时左房功能较差,右心室(RV)功能障碍较严重。
运动时,CpcPH-LHD患者的PAWP与IpcPH-LHD相似,但伴有更严重的RV-PA解耦联,更大的心室相互作用,更严重的心输出量、氧输送和峰值氧消耗障碍。尽管PVR较高,但与IpcPH-LHD和对照组相比,CpcPH参与者发生了更严重的肺充血,这与较低的动脉O2张力、肺泡通气减少、肺O2扩散减少和更大的通气-灌注错配相关。
由此可见,LHD中的肺血管疾病与病理生理特征相关,其特征为运动引起的肺充血、动脉低氧血症、RV-PA解耦、心室相互依赖以及氧输送受损、有氧能力受损。需要进一步的研究来确定新的治疗PH-LHD的方法。
原始出处:
Kazunori Omote.et al.Pulmonary vascular disease in pulmonary hypertension due to left heart disease: pathophysiologic implications.European Heart Journal.2022.https://academic.oup.com/eurheartj/advance-article-abstract/doi/10.1093/eurheartj/ehac184/6633254?redirectedFrom=fulltext
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#生理学#
42
#动脉高压#
40
#病理生理#
46
#病理生理学#
36
#肺血管疾病#
37
#肺动脉高压患者#
39
#ART#
29
#血管疾病#
0
#HEART#
44