在肺动脉高压中Cardiac Effort比较临床和远程6分钟步行测试
2022-07-04 刘少飞 MedSci原创
基于胸部的加速度计可以远程估计6MWT距离吗?与诊所评估相比,远程CE是否比6MWT距离更 与诊所评估相比,远程CE的重现性比6MWT距离更强吗?
六分钟步行测试(6MWT)是一项亚最大运动测试,是肺动脉高压(PAH)治疗研究和风险评估的核心组成部分。除了评估生命体征的设备外,6分钟步行试验只需要一个无障碍的步行空间(最好是30米)。最初的6MWT验证研究以及随后的随访研究显示,对于行走距离大于400米的稳定参与者,重复6MWT距离存在变异性。尽管行走距离大于500米是常规记录,但这种变异性使一些人猜测PAH治疗试验中存在上限效应。另一方面,6MWT距离的减少更容易被接受为临床恶化的标志和一个重要的负面预后信号。为了提高6MWT的可重复性,我们开发了 "Cardiac Effort"(CE),即6MWT期间需要的心脏跳动总量除以6MWT行走距离。这个指标比6MWT距离的变化要小,而且对治疗的变化很敏感。它还与两种不同的右心室(RV)功能评估相关联。 . 目前还没有一个标准化的远程替代方法。Cardiac Effort(CE),即心脏跳动总数除以6分钟步行测试(6MWT)距离(次/米),提高了6MWT的可重复性,并与肺动脉高压(PAH)的右心室功能相关联。
研究问题:
基于胸部的加速度计能远程估计6MWT的距离吗?与临床评估相比,远程CE是否比6MWT距离更具可重复性?
研究设计和方法:
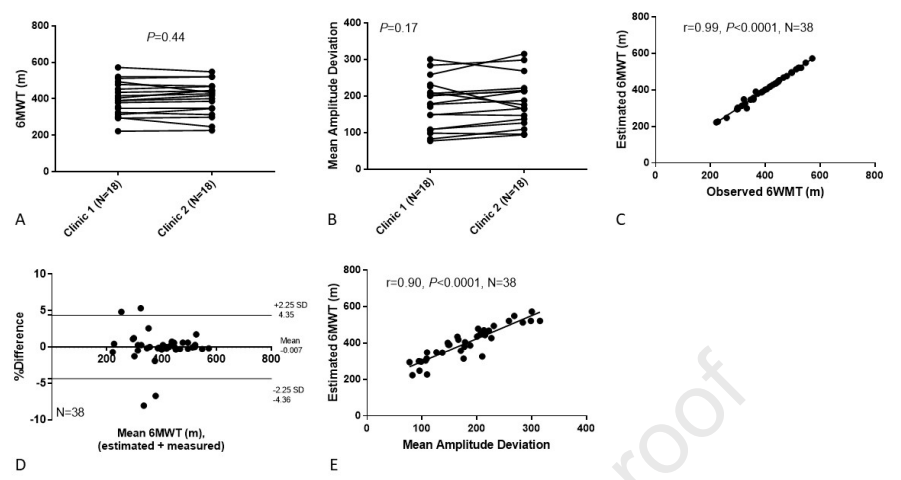
这是一项单中心、前瞻性的观察研究,经IRB批准,于2020年10月至2021年4月完成。接受稳定治疗>90天的第1组PAH受试者在2周内完成4-6次总的6MWT,以评估再现性。第一次和最后一次6MWT是在诊所进行的;2-4次远程6MWT是由参与者自行决定完成的。MC10 Biostamp nPoint传感器佩戴在胸前以测量心率和加速度。两名盲读者使用在诊所或用户定义的路线上获得的加速测量数据来计算圈数。诊所变量和远程变量的平均值被用于Wilcoxson匹配对、Bland-Altman图或Spearman相关系数。
研究结果:
在20名受试者中,使用MC10估计的6MWT与直接测量的6MWT密切相关,r = 0.99,p<0.0001。远程6MWT距离比诊所6MWT距离短,405米(330,464)对389米(312,430),P=0.002。诊所和远程CE之间没有差异,1.75次/米(1.48,2.20)vs 1.86次/米(1.57,2.14),p=0.14。
研究启示:
远程6MWT在用户定义的路线上是可行的;6MWT距离比诊所距离短。由胸部心率和加速器估计的距离计算的CE提供了一个可重复的运动耐力远程评估,与临床测量值相当。
参考文献:
Daniel Lachant, Ethan Kennedy, Blaise Derenze, Allison Light, Michael Lachant, R. James White, Cardiac Effort to Compare Clinic and Remote 6-Minute Walk Testing in PAH, Chest,2022, ISSN 0012-3692,https://doi.org/10.1016/j.chest.2022.06.025.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#DIA#
54
#动脉高压#
35
#步行#
41
学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习
42
精彩评论,需要您登录查看
48