JAHA:心房传导阻滞预测扩张型心肌病患者致命性心律失常
2022-07-20 MedSci原创 MedSci原创
心房传导阻滞是一种易于评估、广泛应用的DCM患者与LTA相关的标志物。心房传导阻滞和AF似乎具有相似的LTA风险。
心房传导阻滞与室上心律失常和卒中有关,甚至与一般人群的心源性猝死相关。心房传导阻滞是否与扩张型心肌病(DCM)中危及生命的心律失常(LTA)和心脏性猝死相关仍不清楚。

近日,心血管疾病领域权威杂志JAHA上发表了一篇研究文章,该研究旨在明确门诊DCM患者心房传导阻滞和LTA之间的关系。
该研究使用了衍生队列(马斯特里赫特扩张型心肌病登记处;N=469)和外部验证队列(乌得勒支心肌病队列;N=321)。心房传导阻滞 (P波持续时间>120毫秒)或房颤(AF)由对研究数据不知情的医生使用数字卡尺进行诊断。
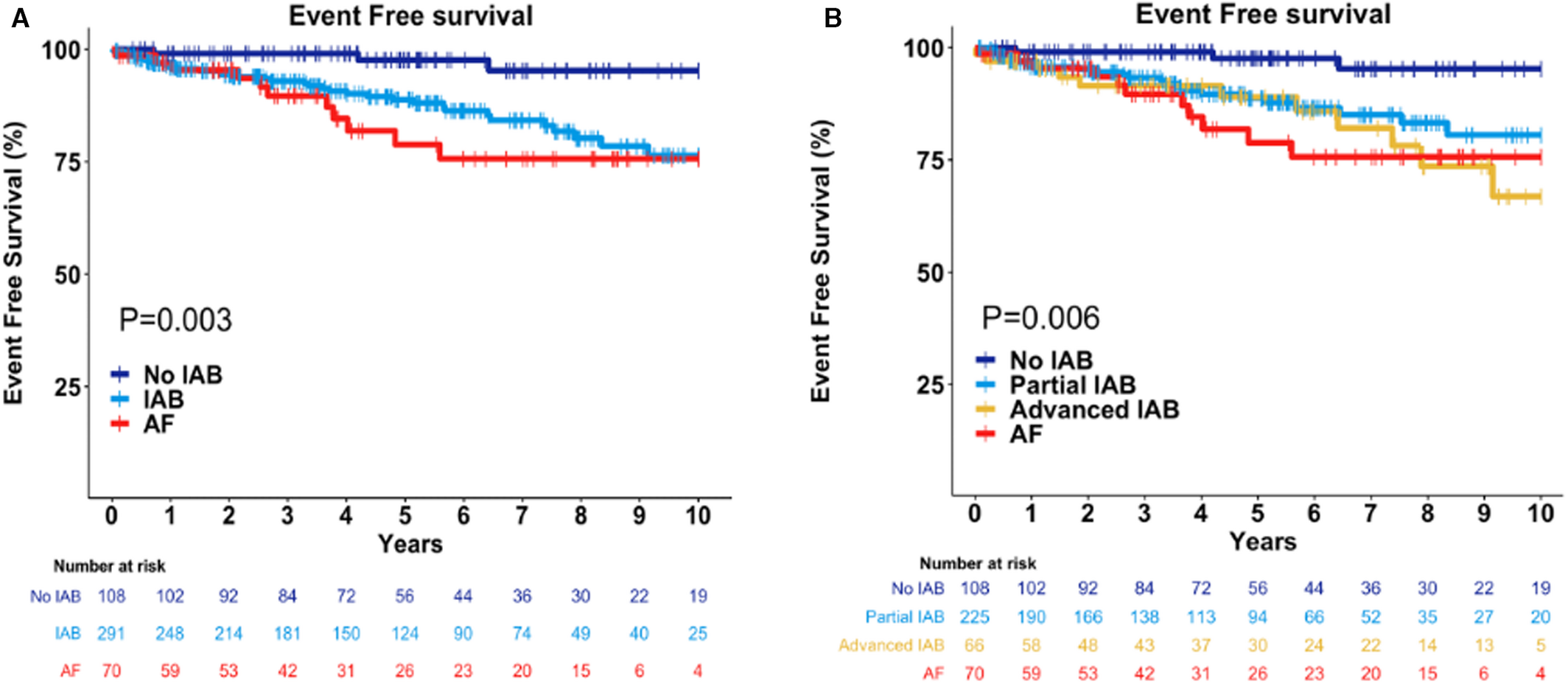
在衍生队列中,分别存有291例(62%)和70例(15%)DCM患者存在心房传导阻滞和AF。49例患者发生LTA(定义为心源性猝死,植入心律转复除颤器或抗心动过速,或血流动力学不稳定的心室颤动/心动过速)(3例无心房传导阻滞, 35例心房传导阻滞, 11例房颤;中位随访时间为4.4年[2.1-7.4])。心房传导阻滞或AF与无心房传导阻滞相比,LTA无生存期分布显著不同(均P<0.01),但心房传导阻滞与AF之间无差异(P=0.999)。这种关联在多变量模型中仍然具有统计学意义(心房传导阻滞: HR为4.8 (1.4-16.1),P=0.013;AF:HR为6.4 (1.7-24.0),p=0.007)。在外部验证队列中,心房传导阻滞或AF患者的生存分布也显著低于无心房传导阻滞患者(P=0.037;P=0.005),但心房传导阻滞与AF之间没有差异(P=0.836)。
由此可见,心房传导阻滞是一种易于评估、广泛应用的DCM患者与LTA相关的标志物。心房传导阻滞和AF似乎具有相似的LTA风险。对DCM患者心房传导阻滞的进一步研究,以及对DCM患者心房传导阻滞的管理是十分有必要的。
原始出处:
Michiel T. H. M. Henkens.et al.Interatrial Block Predicts Life‐Threatening Arrhythmias in Dilated Cardiomyopathy.JAHA.2022.https://www.ahajournals.org/doi/10.1161/JAHA.121.025473
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#扩张#
52
#传导阻滞#
54
#AHA#
47
#肌病#
52
#心房#
61