经导管主动脉瓣置换术(transcatheter aortic valve replacement,TAVR)在我国经过十余年的发展,目前已进入崭新而关键的阶段。2018年,我国首部理论与实践相结合的全流程TAVR临床路径《中国经导管主动脉瓣置换术临床路径专家共识》应时而生,对我国近年来TAVR开展发挥了重要指导作用。首版临床路径问世3年来,TAVR领域在循证证据、应用经验、指南更新、器械研发、术式改良等方面陆续取得重要进展。为进一步紧贴最新证据经验,切实提高我国TAVR能力,推进TAVR规范、安全、健康地发展,特更新此版临床路径专家共识。 1 TAVR患者的临床评估
1. 1 心脏瓣膜病团队的建立(图1)
近年来我国TAVR的实践经验证实,心脏瓣膜病团队对于TAVR的意义重大,是临床路径的真正执行者与实践者。心脏瓣膜团队的作用并不仅限于手术过程,而是涉及评估、治疗到远期康复整个周期的全程指导。完备的心脏瓣膜病团队是早期构建TAVR中心的必备条件,同时也是成熟中心进一步追求TAVR手术更为满意疗效的重要因素。心脏瓣膜病团队需要完成:(1)充分评估患者的临床和解剖适应证及禁忌证,了解患者意愿及经济能力等社会因素;(2)决定治疗方案,制定手术策略并评估其可行性,考虑可能出现的并发症及处理方案;(3)实施TAVR治疗并保障围术期管理质量;(4)远期随访康复指导。

1. 2 临床评估要点
临床评估是以患者主动脉瓣疾病干预指征为核心的临床综合评估,其重点包括TAVR的适应证、手术方式选择及禁忌证三大步骤。瓣膜置换的适应证和预期获益主要通过评估患者超声心动图及临床症状,确定主动脉瓣疾病的严重程度及风险分期,从而确认干预时机及获益。而在外科或介入手术方式选择方面,由于近年来TAVR外科风险低危化进程的进展,目前外科风险评分评估地位较前下降,不再是衡量患者主动脉瓣治疗方式的独立指标。以解剖学风险为基础结合临床综合性评估(日常生活能力评定、心理评估、营养状态评估、认知功能评估、虚弱评估、运动技能评估、神经系统功能评估)可更全面描述患者个体化情况,协助治疗方式的选择。禁忌证评估方面则需要根据患者临床资料的全面采集了解有无急性心肌梗死、流出道梗阻、左心血栓形成或解剖不适合TAVR的情况,同时还需要进行无效性评估,考量术后预期寿命及生活质量改善的可能。
1. 3 适应证及禁忌证的指南更新
近年来TAVR指南更新的重点是适应证的拓展和干预方式的转变。由于低危患者TAVR循证证据和经验的积累,2020年美国瓣膜性心脏病患者管理指南不再按外科危险分层作为主动脉瓣狭窄(aortic valve stenosis,AS)患者手术方式推荐,而是强调预期寿命、人工瓣膜耐久性以及解剖特点作为选择外科主动脉瓣置换术(surgical aortic valve replacement,SAVR)还是TAVR的主要考量因素:年龄>80岁或预期寿命<10年的患者首选经股动脉路径(trans-femoral,TF)TAVR;年龄65~80岁、无TF TAVR禁忌证的有症状患者,建议医师和患者共同决策,选择SAVR或TF TAVR;如治疗后预期生存时间>12个月且生活质量可接受,TAVR是任何年龄段有症状、手术高危或有手术禁忌患者的首选。2021年欧洲心脏瓣膜病管理指南则同样推荐SAVR应用于外科低危的年轻患者(<75岁)或不适合TF TAVR的患者,而外科高危且>75岁的高龄患者或不适合外科手术的患者首选TAVR治疗。该指南再次强调干预方式选择依赖于临床评估团队和根据患者个体化的临床和解剖特点共同决策。《经导管主动脉瓣置换术中国专家共识(2020更新版)》指出,外科中高危患者为TAVR的绝对适应证,外科手术低危且年龄≥70岁、二叶式主动脉瓣为TAVR的相对适应证。
基于近年来国内外指南和专家共识,TAVR的适应证和禁忌证更新如下。
绝对适应证:(1)重度AS,超声心动图示跨主动脉瓣血流速度≥4 m/s,或跨主动脉瓣平均压差≥40 mmHg(1 mmHg=0.133 kPa),或主动脉瓣口面积≤1.0 cm2,或有效主动脉瓣口面积指数≤0.6 cm2/m2。对于低压差-低流速患者,根据左心室射血分数是否正常需进行进一步评估(如行多巴酚丁胺试验)明确狭窄程度。(2)患者有AS导致的临床症状(分期D期)或心功能减低,包括左心室射血分数<50%及纽约心脏病协会(New York Heart Assdciation,NYHA)心功能分级Ⅱ级以上。(3)存在外科手术禁忌或高危或存在其他危险因素,如胸部放射治疗后、肝功能衰竭、主动脉弥漫性严重钙化、极度虚弱等。(4)主动脉根部及入路解剖结构符合TAVR(特别是TF TAVR)要求。(5)三叶式主动脉瓣。(6)术后预期寿命>1年。(7)外科主动脉生物瓣膜毁损且再次外科手术高危或禁忌的患者。
相对适应证:(1)外科手术中、低危且年龄≥70岁;(2)二叶式AS,因目前国内自膨胀瓣膜及球囊扩张瓣膜数据均提示经过充分的解剖形态评估和正确的手术策略,可达到不劣于三叶瓣的临床结果,可在有经验的中心以及术者中开展;(3)60~69岁患者经过临床综合评估认为更适合行TAVR手术者;(4)单纯严重主动脉瓣反流(aortic valve regurgitation,AR),外科手术禁忌或高危,预期治疗后能够临床获益,解剖特点经过充分评估适合TAVR手术者首选经心尖路径的成熟器械,TF TAVR尚证据不足,仅可在有经验的中心以及术者中进行探索性尝试。
禁忌证:(1)左心室内新鲜血栓;(2)左心室流出道严重梗阻;(3)急性心肌梗死;(4)主动脉根部解剖形态不适合行TAVR治疗;(5)存在其他严重合并症,即使纠正了瓣膜狭窄仍预期寿命不足1年。
2 TAVR围术期的影像学评估
准确的影像学评估是TAVR成功的基础。术前评估的目的是筛选符合TAVR适应证的患者及恰当的器械型号及手术入路;术中旨在评估瓣膜的准确定位释放及功能评估;术后旨在评估是否有并发症及治疗效果。不同的影像学评估手段各有优势。
2. 1 计算机断层显像(computer tomography,CT)评估
CT在TAVR术前评估、术中指导以及术后随访中处于核心地位,而且是术前人工瓣膜及入路选择的“金标准”。
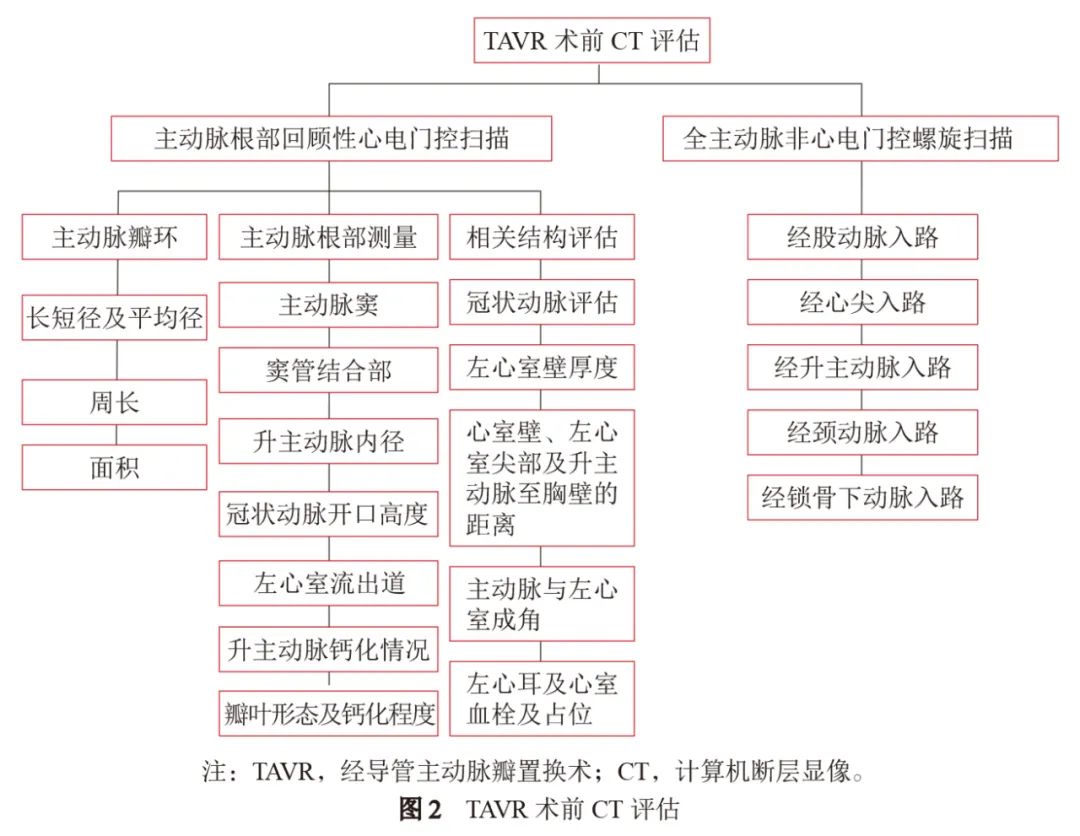
术前测量评估:需要有经验的影像核心实验室通过专业软件对CT图像进行分析,主要观察主动脉根部和入路的形态学特征(图2)。术者需要熟练掌握影像评估方法并对结果进行充分解读及个体化分析,可根据图像结果识别解剖难度、评估风险并制订正确手术策略。
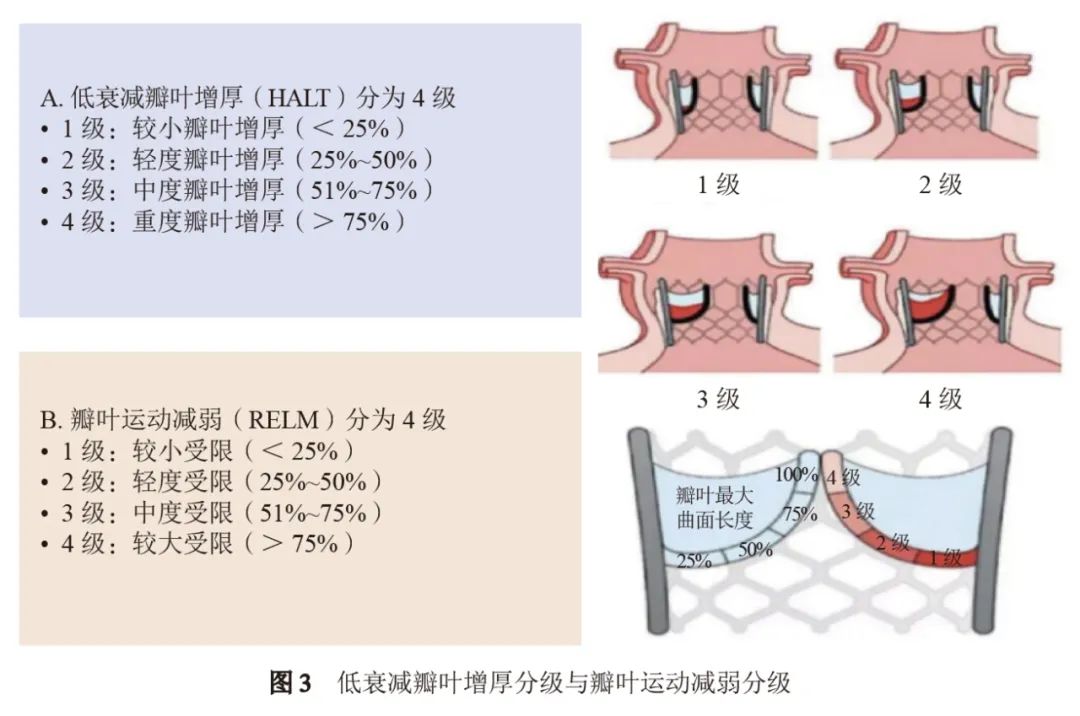
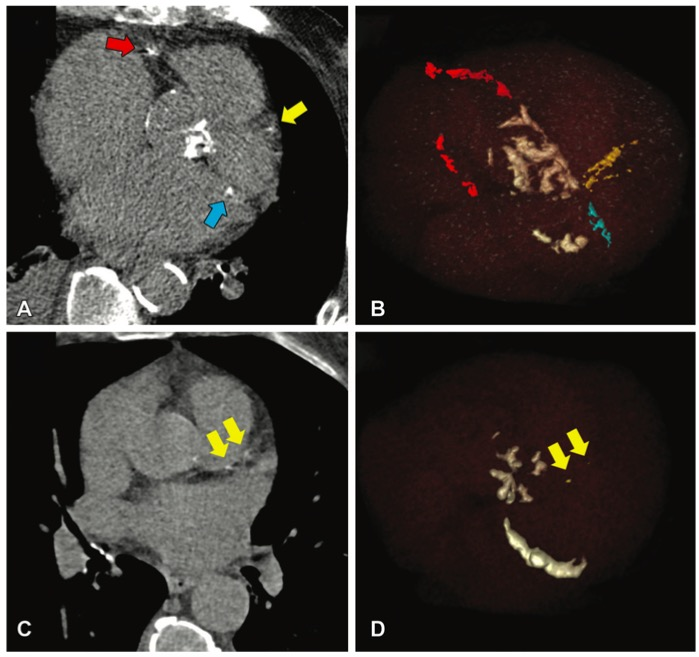
术中、术后CT评估:通过CT可对导丝跨瓣及最佳释放角度进行预测,以减少术中X线的辐射剂量及对比剂的使用。术后通过CT可判断瓣膜置入位置及深度、瓣架膨胀程度及椭圆率,通过舒张期及四维(4 dimension,4D)CT动态观察瓣叶,可了解有无异常瓣叶增厚或血栓形成来评价器械远期效果或制订抗凝抗栓策略,目前高分辨4D CT是诊断导管置入瓣膜血栓形成的“金标准”,主要影像学特征是不同程度的低衰减瓣叶增厚(hypo-attenuated leaflet thickening,HALT)征和瓣叶运动减弱(reduced leaflet motion,RELM)(图3)。
2. 2 超声心动图评估
术前评估:通过经胸超声心动图(transthoracic echocardiography,TTE)可以对整体心脏及主动脉瓣的形态学与功能学状态进行准确判定,重要的参数包括房室内径、室壁厚度、左心室射血分数,主动脉瓣形态学参数包括瓣环内径、瓣叶数目、钙化病变程度,功能学参数包括有效瓣口面积、峰值流速、平均/最大跨瓣压差等。对于低压差-低流速患者可进行多巴酚丁胺试验进一步检查。
术中监测及术后随访:术中监测方案根据患者采用麻醉方案不同可以选用不同方式[经食管超声心动图(transoesophageal echocardiography,TEE)或TTE]。术中超声心动图对于瓣膜置入后即刻评估瓣膜功能及心脏综合评价,尤其是主动脉瓣瓣周反流的定位、定量有优势。患者术后TTE随访早期的观察重点在于有无急性或亚急性并发症,如心包积液、主动脉根部血肿、瓣膜位置功能等;远期随访重点在于心脏整体、人工瓣膜形态及功能状态的评估。
3 规范化TAVR流程
3. 1 场地及器械要求
建议在具备复合手术功能的介入导管室或手术室进行,应同时具备血管造影设备和外科手术条件,空气层流达到心外科手术要求。设备要求:血管造影机C型臂、血流动力学监护设备、麻醉机及体外循环机需满足心外科手术要求。同时需配备除颤仪、高压注射器、超声心动设备及临时起搏器等,各型号鞘管(4~22 F)、导管、导丝、各型号球囊(冠状动脉、外周及主动脉扩张球囊)、冠状动脉及外周血管相关支架等。手术室内人员应各司其职,合理安排站位。
3. 2 麻醉的选择
麻醉方式包括:局部麻醉(local anesthesia,LA);镇静或监护麻醉(monitored anesthesia care,MAC),在保持一定镇静深度(意识可消失)的基础上,辅以局部麻醉药完成各项有创操作及手术,术毕可直接唤醒;全身麻醉(general anesthesia,GA),维持一定的镇静、镇痛和肌肉松弛,行气管插管、机械通气,完成手术。麻醉方式的选择主要依据患者本身状态、术者和麻醉医师、TAVR的入路等。建议各中心早期开展可适当选择全身麻醉为主,经验累积后可根据情况调整麻醉的方式。
3. 3 入路的选择和建立
根据术前影像学评估选择合适的入路,目前以我国的经验80%以上可以选择TF。如存在股动脉血管管腔严重狭窄、血管严重迂曲以及重度钙化等,可以选择其他入路,建议由具备血管外科支持,并且经验丰富的中心来完成。行TF的患者,可以选择穿刺或者切开,建议术前细致评估穿刺位置,并在超声引导下进行穿刺。也可使用微穿刺装置进行主入路血管穿刺或副入路穿刺后,在造影指导下完成主入路穿刺并预置预缝合装置进行缝合。
3. 4 瓣膜的选择
目前我国大陆共有4款TF的TAVR瓣膜、1款经心尖入路的TAVR瓣膜上市,包括球囊扩张式瓣膜、自膨胀式瓣膜两大类,其中已有3款升级为可回收系统。进行瓣膜选择时应基于术前CT综合瓣膜的分型、瓣膜钙化分布、冠状动脉堵塞风险、永久起搏器植入可能性、瓣环破裂风险、生物瓣膜不匹配等,结合患者血管入路情况,必要时结合术中球囊扩张的结果,并根据每一款瓣膜的特性,做到个体化选择。
3. 5 瓣膜置入前的准备
临时起搏电极植入:快速起搏用于球囊预扩张或瓣膜释放过程,以减少瓣膜移位。起搏电极推荐使用漂浮电极导线,可降低植入难度及减少心肌穿孔的概率。随着极简式TAVR观念的推广,左心室导丝起搏的应用逐渐增加,应用时仍需评估患者的起搏器植入风险,对于高风险患者仍建议常规植入临时起搏器,必要时术后留置72 h。
跨瓣:术前通过多排CT(multidetector CT,MDCT)选择最佳的跨瓣角度,通常选取可充分观察瓣叶、钙化团块分布与瓣口开闭情况的角度。跨瓣时的核心步骤是逐步有序调整导管轴向及高度,同时反复尝试操作导丝跨瓣,直至导丝头端进入瓣口。跨瓣困难时应更换不同指引导管进行尝试。跨瓣成功后需要交换为超硬导丝进入左心室以支撑球囊和瓣膜的输送,应特别注意超硬导丝前端的形态和位置,避免术中造成心室壁损伤甚至穿孔。
瓣膜释放角度的选择:术前通过MDCT对器械释放角度进行预测,结合术中主动脉根部造影,确定瓣膜最佳释放角度。目前常用的方法有右窦中心法则、双S曲线以及窦部重叠(cusp-overlap)技术。
预扩张:球囊预扩张与否需要综合考虑下列关键因素:(1)瓣膜钙化增生程度是否影响器械通过性或导致人工瓣膜移位;(2)是否需要球囊扩张观察球囊腰部及根部造影反流量辅助选择瓣膜型号。目前我国大多数患者需要进行球囊预扩张,选择球囊型号时应参考术前CT结果。球囊扩张时需要进行快速起搏,同时进行根部造影,观察球囊膨胀效果、反流情况以及冠状动脉灌注情况。对于不具备瓣膜置入条件的中心,如果行急诊球囊主动脉瓣膜扩张抢救患者,球囊扩张宜在超声心动图或者CT分析支持下,从小型号球囊开始,避免造成根部破裂及瓣膜大量反流。
3. 6 瓣膜的输送、定位及释放
输送:瓣膜跨主动脉弓时,同时观察到弓部情况以及左心室导丝情况,助手协助调整导丝,让瓣膜尽量平顺跨越主动脉弓。瓣膜跨瓣时,需要向前推瓣膜的同时保持特硬导丝稳定性,如果因瓣膜钙化或升主动脉扩张导致瓣膜跨瓣困难,应及时使用抓捕器辅助跨瓣,切勿暴力操作导致升主动脉夹层或心脏破裂。
定位及释放:不同瓣叶结构、瓣膜型号对起始定位的高度要求有所不同,应通过术前CT分析确定人工瓣膜的锚定区和封堵区。根据不同瓣膜设计规划置入深度,在主动脉根部造影下进行释放。瓣膜释放过程中可能需要应用快速起搏,根据瓣膜类型以及释放策略不同,起搏频率常规120~220 次/分。
3. 7 释放后评估及并发症的处理
术后应观察血流动力学情况,通过超声心动图和主动脉根部造影来评估瓣膜的位置及反流情况,同时观察二尖瓣、左心室功能以及心包情况,并结合患者的生命体征、临床症状,快速识别并发症。术后常见的并发症总结如下:(1)卒中:目前我国各大中心显示有症状的卒中发生率约为1%,TAVR后24 h是高危期。采用术中脑保护装置可能降低卒中发生率,但目前仍缺乏大规模临床研究数据支持。(2)传导阻滞:TAVR后出现新发传导阻滞主要与心脏传导束系统受到人工瓣膜机械压迫相关,应避免使用过大的人工瓣膜及置入位置过深,对于束支阻滞的高危患者可考虑采用球囊扩张式瓣膜。(3)血管并发症:血管并发症是TF TAVR的常见并发症,发生比例较高,但随着输送装置径线的不断缩小,血管并发症的发生率有进一步降低趋势。避免血管并发症的主要方法为加强术前评估,选择合理的切开或预缝合方式,必要时评估其他入路。如出现血管并发症可通过球囊封堵、覆膜支架置入及外科手术予以补救。(4)心肌梗死:术中导致心肌梗死的最常见原因为急性冠状动脉闭塞。在术前评估时应特别注意冠状动脉开口高度、窦部容积、瓣叶增厚及钙化情况以及人工瓣膜与冠状动脉开口的关系。术中冠状动脉闭塞高危患者可通过球囊预扩张同时根部造影观察冠状动脉灌注情况,或采用导丝进行冠状动脉保护。(5)瓣膜反流:人工瓣膜中心性反流多源于瓣膜位置和膨胀不良,必要时可通过球囊后扩张改善。TAVR后的瓣周反流是常见并发症之一,发生率明显高于SAVR。既往研究证实中量及以上的瓣周反流会影响临床结果及预后。预防瓣周反流措施包括术前细致的影像评估,选择适合的瓣膜型号;术中选择新一代的可回收或具有“外包裙边”的瓣膜;精确定位置入深度。
其他常见并发症包括:(1)急诊外科开胸;(2)计划外的体外循环支持;(3)室间隔穿孔;(4)心脏压塞;(5)二尖瓣功能损伤;(6)感染性心内膜炎;(7)瓣膜移位;(8)瓣膜血栓;(9)瓣中瓣置入;(10)出血;(11)急性肾损伤。
3. 8 急诊TAVR流程
随着我国TAVR近年的发展,由于部分患者术前呈现危重状态,急诊TAVR的探索随之逐渐进入临床实践。开展急诊TAVR的心脏团队需兼备成熟的手术技术与急危重症抢救经验。TAVR患者需要进行急诊干预的主要适应证包括:合并心源性休克,合并有持续性室性心动过速或发生心室颤动等恶性心律失常,药物难以改善需要器械循环辅助装置的严重心肌缺血或慢性心力衰竭症状,在TAVR评估及手术前阶段出现血流动力学崩溃接受心肺复苏的患者。急诊TAVR患者可能因病情严重无法完善术前CT评估且病情危重,根据目前国内外经验对流程做以下建议:对血流动力学不稳定者或病情危重者,建议术前置入机械循环辅助装置,优选体外膜肺氧合(extracorporeal membrane oxygenation,ECMO),次选主动脉内球囊反搏(intra-aortic balloon pump,IABP)进行辅助;术中首选全身麻醉方式,TEE评估主动脉根部结构;根据血管超声及术中造影结果,优选TF;根据超声心动图选择预扩张球囊型号,术中预扩张时应特别关注冠状动脉灌注以及反流量情况,必要时可选择小球囊续贯扩张,避免大量反流所致循环不稳定;根据术中根部造影和球囊扩张造影(balloon sizing)选择人工瓣膜型号;术后患者建议在监护病房进行过渡治疗(图4)。

3. 9 极简式TAVR流程
极简式TAVR是目前国内外探索TAVR流程中非常重要的方向,在适合的患者中实施,其有效性和安全性不劣于常规TAVR手术方式,且创伤更小、操作更简单、住院时间更短,也更易推广。极简式的简化部分应该着重于手术流程,而术前适合极简式患者的评估则应该比常规TAVR更为细致准确。参照标准化方案TAVR前评估流程且需要完备以下条件:(1)具备合适的血管入路;(2)根部解剖条件佳,无特殊解剖因素相关并发症风险(如冠状动脉风险过高、瓣环破裂风险高等);(3)无慢性疼痛,配合度佳;(4)TTE声窗条件好;(5)一般情况好,可以平卧。围术期管理及手术操作中主要作如下简化:(1)手术地点可选择介入导管室;(2)使用TTE进行术中辅助;(3)采用局部麻醉+镇静或单纯局部麻醉方式;(4)避免有创动脉通路和右心导管置入;(5)条件适合者可不予导尿;(6)在外周血管超声引导或对侧造影指导下穿刺主入路股动脉,避免外科切开;(7)条件适宜患者采用经桡动脉副入路;(8)条件适宜患者可采用左心室支撑导丝起搏(需评估患者永久起搏器植入风险);(9)主入路预埋两把血管缝合器方式闭合;(10)瓣膜置入后给予鱼精蛋白中和部分肝素,以促进术后4 h患者能够早期活动;(11)早期撤除有创管路,鼓励患者早期活动,促进患者更快地恢复到基线的功能状态。根据临床、超声心动图、心电检查、实验室检查评估术后情况,可较常规TAVR更早出院。
3. 10 单纯AR的TAVR治疗
单纯AR特指不伴有狭窄和钙化增厚的患者,由于瓣环及瓣叶没有钙化缺乏锚定、瓣环较大且解剖变异性大、通常合并有升主动脉扩张等,使用自膨胀瓣膜系统行TAVR治疗单纯AR难度很高,并不作为常规推荐。目前我国仅有经心尖入路的J-Valve人工主动脉瓣膜被批准用于AR的TAVR治疗。经心尖入路主要应避免损伤冠状动脉,缝制荷包;顺行跨瓣后置入加硬导丝;将J-Valve输送装置放至升主动脉后回撤窦底落位释放。部分有经验的中心尝试在严格筛选后的患者中开展TF自膨胀瓣膜的置入,其核心筛选条件包括患者外科手术禁忌或极高危且解剖条件具备多径线锚定可能,主要手术步骤中通常跨瓣较为简单且无需预扩张,对于瓣膜型号选择尚无统一标准,推荐按照瓣环尺寸增加10%~20%作为参考;推荐左右窦重叠角度以充分展开流出道,瓣膜释放起始位置一般稍微低位(2~4 mm),需参考瓣环和流出道长度决定,不推荐0位或者高位释放,可回收瓣膜优选;瓣膜释放先慢后快,控制节奏寻求锚定。目前单纯AR的TF TAVR尚处于探索早期,需特别慎重选择。
3. 11 TAVR+经皮冠状动脉介入治疗(percutaneous coronary intervention,PCI)流程
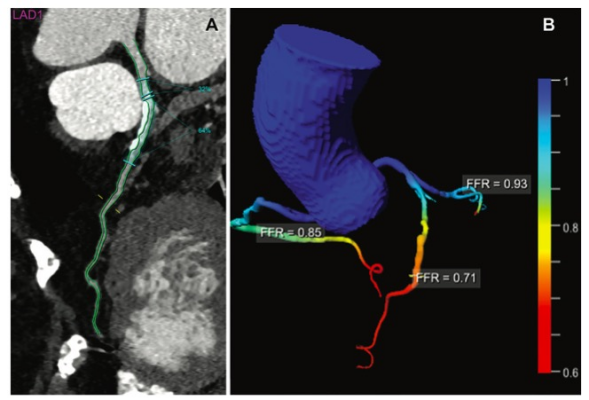
AS合并冠心病(coronary artery disease,CAD)患者在临床常见。随着TAVR技术的成熟,TAVR+PCI的介入治疗组合方式已成为该人群的治疗方式之一。2021欧洲心脏瓣膜病管理指南建议TAVR患者合并冠状动脉近端狭窄>70%时可采用PCI方式进行干预。目前TAVR后进行PCI因冠状动脉入路难度增加不作为常规推荐,而TAVR术前行PCI或术中进行一站式PCI两种组合哪个更为优越尚待证实。一站式TAVR+PCI应在有经验的中心开展,早期应选择简单组合进行处理,建议进行预先跨瓣置入猪尾导管;对于合并左主干病变、多个靶病变、需要旋磨以及二叶式主动脉瓣的复杂PCI+TAVR一站式治疗的患者,应特别注意基础心功能及肾功能,避免多个难点进行组合导致手术难度过大、时间过长从而增加风险;手术过程中对于冠状动脉病变复杂及基础心功能状态不佳患者,应充分评估其麻醉方式及是否需要左心辅助装置。TAVR后球囊扩张式瓣膜再次进入冠状动脉相对简单,而自膨胀式瓣膜操作较为困难。TAVR中冠状动脉闭塞风险高的患者需进行细致的预判,推荐采用导丝保护及选择“开口”或“烟囱”支架保护技术以减少风险。
3. 12 TAVR+左心耳封堵术(left atrial appendage closure,LAAC)流程
TAVR合并心房颤动患者中,可根据血栓及出血评分评估LAAC指征适合患者。根据TAVR患者术前常规根部CT评估左心耳血栓形成情况,对于无血栓形成患者可考虑TAVR+LAAC一站式手术流程:在全身麻醉并TEE指导下完成TAVR后同台行LAAC治疗。对于存在左心耳血栓患者可先行TAVR后抗凝3个月再评估LAAC治疗方案。一站式术后常规监护,术后次日及第3天分别复查TTE。术后根据患者个体化情况制订抗凝抗栓方案,术后第45天及之后按时常规随访,观察症状+头颅CT随访卒中再发情况,术后第45天、12个月时通过TEE观察封堵器是否完全封闭左心耳,有无器械表面血栓形成。术后建议双联抗血小板6个月后终身单抗血小板治疗。
3. 13 外科生物瓣膜毁损的瓣中瓣技术
由于二次开胸外科手术风险较高,TAVR的瓣中瓣技术具备独特优势。TAVR治疗主动脉瓣外科生物瓣膜毁损重要步骤包括:(1)术前明确外科生物瓣膜的类型与型号,与CT结果互相印证,并需要特别了解冠状动脉开口阻塞风险,选择合适TAVR瓣膜类型及型号;(2)除非毁损形式为重度狭窄,多数采用不预扩张直接释放介入瓣膜,而对于采用自膨式瓣膜行TAVR时,若术后认为形态差、跨瓣压差高等情形存在时,可选择球囊进行适当的后扩张;(3)应注意主动脉瓣生物瓣膜毁损时,如果首次外科开胸手术的瓣膜尺寸较小,特别外科生物瓣膜内径小于17 mm时,建议考虑非顺应强力球囊打断原有外科生物瓣环,否则置入TAVR瓣膜型号过小或膨胀不良容易影响压差及瓣膜使用寿命。
4 围术期综合管理及术后康复随访
4. 1 TAVR患者围术期管理及随访康复策略
TAVR患者术后管理主要包括围术期管理、术后中长期随访及远期康复。在术后应根据麻醉方式及入路情况,酌情于重症监护室进行过渡或于普通病房进行治疗,进行精细的循环容量管理,疼痛管理,呼吸系统、神经系统及消化系统的综合管理。在容量管理方面,建议根据患者基础心肺能力及储备功能等特点采取个体化补液方案,需根据患者临床症状、体征、X线胸片、B型利钠肽(B-type natriuretic peptide,BNP)及中心静脉压(central venous pressure,CVP)等指标调整。其他监测重点包括心律的变化(起搏器评估)、呼吸道感染、穿刺点出血、急性肾损伤、脑血管事件等(具体见3.7节“释放后评估及并发症的处理”)。结合Popular-TAVI研究结果,对于有抗凝适应证者(如心房颤动、血栓栓塞等),建议长期应用维生素K拮抗剂抗凝,非维生素拮抗剂类抗凝药因证据有限目前不予推荐;对于无抗凝适应证者,建议直接单种抗血小板药物长期治疗。TAVR后康复包括围术期康复、门诊康复和居家康复。围术期康复包括术前预康复、术后监护病房康复、术后普通病房康复。术后康复主要根据患者整体情况和穿刺置管条件,个体化评估运动康复方案。完善患者在院相关检查、体能及运动耐力测试等相关评估后,结果良好、状态平稳者可于术后2~5 d内出院,并于术后1个月、6个月及12个月完成常规门诊随访,包括常规实验室检查、超声心动图及其他常规功能检查,其中6个月及12个月可根据患者经济能力建议复查主动脉根部CT,评估人工瓣膜形态位置及亚临床血栓形成情况,调整抗栓方案,如发现亚临床血栓形成建议改为维生素K拮抗剂抗凝后再行影像学检查评估。术后管理团队、评估团队、康复团队联合心内科医师可通过门诊随访为主,微信、电话为辅,及时获悉患者不良事件,共同完成术后中长期随访及评估,及时处理并发症,合理调整药物,术后康复指导等。建议术后3个月于康复门诊继续进行康复训练,根据情况制订长期家庭康复计划,定期复诊,修正心脏康复处方。
4. 2 特殊类型患者随访要点
对于术前伴有升主动脉扩张的患者,需密切监测升主动脉内径扩张程度及速度,适当增加影像学评估频率(每3~6个月评估一次超声心动图或CT),综合包括心外科医师的意见,考虑干预与否及方式。对于瓷化主动脉或主动脉严重动脉粥样硬化患者,出院时加强宣教,及时纠正高血糖、高血压、血脂异常等心血管不良事件危险因素。必要时增加外周血管和脑血管评估内容。对于TAVR同期行冠状动脉支架置入患者应密切关注冠状动脉病变的进展情况,规范口服抗血小板药物的使用情况,综合评估瓣膜和冠状动脉的治疗策略。
5 结语
TAVR作为目前炙手可热的瓣膜性心脏病介入领域最为成熟的技术,正展现出优越的先进性和强大的生命力。更加广泛的适应证、更加可靠的手术器械、更加优化的操作流程、更加过硬的循证证据均有力推动了TAVR的广泛应用。我国TAVR事业蓬勃发展,中国数据和经验正逐步走向国际舞台。希望本临床路径的更新可以更好地助力我国TAVR技术健康、规范开展,开拓中国TAVR特色创新之路,保障我国广大瓣膜性心脏病患者生命健康。
写作组成员:
王墨扬(中国医学科学院阜外医院),牛冠男(中国医学科学院阜外医院),潘文志(复旦大学附属中山医院),刘先宝(浙江大学医学院附属第二医院),李捷(广东省人民医院),宋光远(首都医科大学附属北京安贞医院),李飞(空军军医大学西京医院),尚小珂(华中科技大学同济医学院附属协和医院),朱政斌(上海交通大学医学院附属瑞金医院),张龙岩(武汉亚洲心脏病医院),张海波(首都医科大学附属北京安贞医院),姜正明(郑州大学第一附属医院),房芳(首都医科大学附属北京安贞医院),科雨彤(首都医科大学附属北京安贞医院),徐磊(首都医科大学附属北京安贞医院),弥守玲(复旦大学附属中山医院),许海燕(中国医学科学院阜外医院),卢志南(首都医科大学附属北京安贞医院),袁素(中国医学科学院阜外医院),叶蕴青(中国医学科学院阜外医院),于子凯(中国中医科学院西苑医院),冯天捷(中国医学科学院阜外医院),姚晶(首都医科大学附属北京安贞医院),王宇彬(首都医科大学宣武医院),张倩(中国医学科学院阜外医院),周政(中国医学科学院阜外医院),陈阳(中国医学科学院阜外医院),张纯(首都医科大学附属北京安贞医院),武德巍(首都医科大学附属宣武医院),杨剑(空军军医大学西京医院),李喆(中国医学科学院阜外医院),孟欣(空军军医大学西京医院),王彬成(中国医学科学院阜外医院),王建德(中国医学科学院阜外医院),张海彤(中国医学科学院阜外医院),张洪亮(中国医学科学院阜外医院),赵庆豪(中国医学科学院阜外医院),赵晟(中国医学科学院阜外医院),赵振燕(中国医学科学院阜外医院)
高润霖(中国医学科学院阜外医院),葛均波(复旦大学附属中山医院),韩雅玲(中国人民解放军北部战区总医院)
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#置换#
48
#专家共识#
42
#主动脉瓣#
42
#主动脉瓣置换术#
59
#主动脉#
35
#经导管#
54
#经导管主动脉瓣置换#
56
#置换术#
38
学习#学习#
62