Atherosclerosis:预防动脉粥样硬化 每天睡几个小时更合适?
2018-08-14 徐钰琦 环球医学
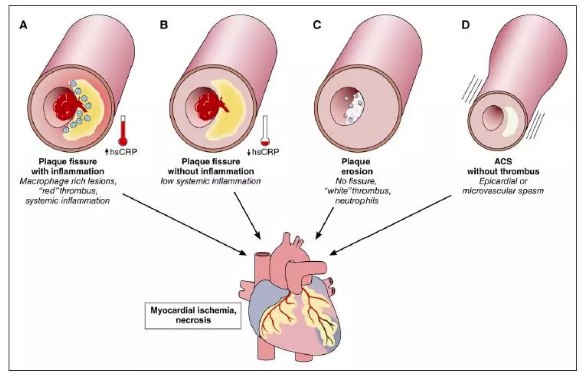
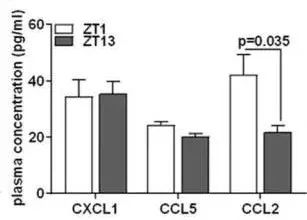
2018年7月,发表于《Atherosclerosis》上的阿拉贡工人的健康研究(AWHS),考察了睡眠时间与亚临床动脉粥样硬化的相关性。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#Sclerosis#
37
学习了谢谢分享!!
60
#粥样硬化#
36
#ROS#
31
学习了谢谢分享!!
64
学习了
65
不错的文章值得推荐一下
60
不错的文章值得拥有
54