JAHA:主动脉瓣置换术患者中性粒细胞与淋巴细胞比值的临床意义
2022-06-05 MedSci原创 MedSci原创
基线NLR升高与TAVR或SAVR后死亡率和再住院增加独立相关。TAVR或SAVR后观察到的NLR降低与患者预后改善相关。
全身性炎症和心力衰竭(HF)之间有很强的相互关联和潜在的协同作用。而外周组织炎症介质可以影响HF的发生和发展,HF患者的压力负荷过载和剪切应力可能导致心肌促炎细胞因子释放。中性粒细胞与淋巴细胞比值(NLR)作为全身性炎症的标志,在包括心力衰竭在内的几种慢性疾病状态下,NLR与较差的患者预后相关。然而,对于经导管或外科主动脉瓣置换术(TAVR或SAVR)治疗的主动脉瓣狭窄的患者,随访期间基线NLR升高或NLR水平变化对患者预后的影响目前尚未明确。

近日,心血管疾病领域权威杂志JAHA上发表了一篇研究文章,在主动脉导管置换术(PARTNER)I、II和S3试验/注册的5881例严重主动脉狭窄患者中,他们接受了TAVR或SAVR治疗,且这些患者NLR可用(中位NLR[Q1,Q3]为3.30[2.40,4.90]);平均NLR为4.10;范围为0.5-24.9),并将NLR作为连续变量和分类变量三分位数进行了评估(低NLR≤2.70,n=1963;中间值NLR为2.70-4.20,n=1958;高NLR≥4.20,n=1960)。
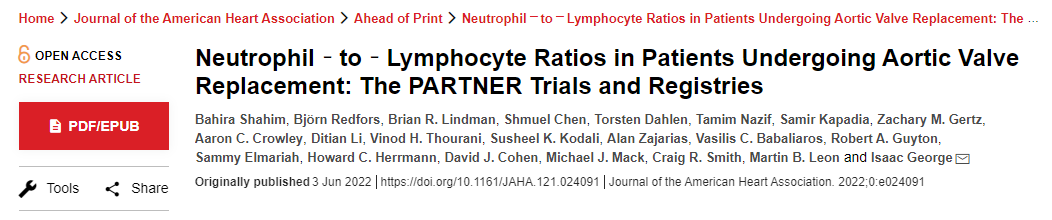
没有患者在基线时出现已知的感染。与低NLR组相比,高基线NLR与3年死亡或再住院风险增加相关(58.4% vs 41.0%;调整后的风险比[aHR]为1.39;95%置信区间为1.18-1.63;P<0.0001),且与治疗方式无关。
在接受TAVR和SAVR治疗的患者中NLR从基线至2年之间有所下降。基线至1年期间观察到的NLR降低1个单位与1-3年期间死亡或再住院风险降低相关(aHR为0.86;95%置信区间为0.82-0.89;P<0.0001)。
由此可见,基线NLR升高与TAVR或SAVR后死亡率和再住院增加独立相关。TAVR或SAVR后观察到的NLR降低与患者预后改善相关。
原始出处:
Bahira Shahim.et al.Neutrophil‐to‐Lymphocyte Ratios in Patients Undergoing Aortic Valve Replacement: The PARTNER Trials and Registries.JAHA.2022.https://www.ahajournals.org/doi/10.1161/JAHA.121.024091
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#置换#
48
#AHA#
57
#中性粒细胞#
66
#淋巴细胞#
64
#主动脉瓣#
49
#主动脉瓣置换术#
47
#主动脉#
44
#置换术#
51