Br J Cancer:英国斯隆项目:11337例乳腺导管原位癌(DCIS)筛查以及后续事件的病理特征研究
2020-11-23 xiaozeng MedSci原创
乳腺导管原位癌(DCIS)是一种异质性疾病,目前在乳腺癌筛查中被越来越多地诊断出来。英国国家卫生服务机构乳腺癌筛查计划(NHS BSP)每50年邀请50-70岁的女性参与两次乳腺癌筛查。
乳腺导管原位癌(DCIS)是一种异质性疾病,目前在乳腺癌筛查中被越来越多地诊断出来。英国国家卫生服务机构乳腺癌筛查计划(NHS BSP)每50年邀请50-70岁的女性参与两次乳腺癌筛查。
为纪念乳腺癌病理学家约翰·斯隆(John Sloane)教授而建立的Sloane项目是一项前瞻性队列研究,旨在研究在NHS BSP中筛查到的非侵润性乳腺癌患者的临床、影像学和病理学特征,护理方式以及患者的结局。
该研究是一项全国性前瞻性队列研究,通过筛查2003年至2012年期间诊断为DCIS的患者,并对患者的病理、后续管理以及结果进行比较。
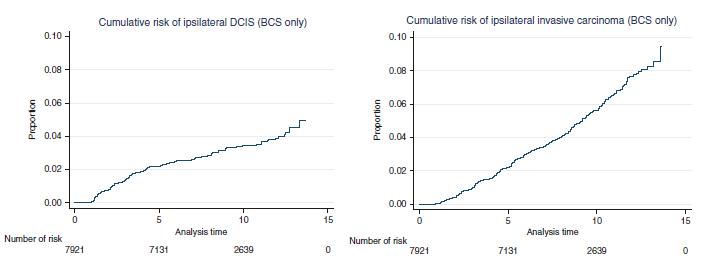
接受保乳手术(BCS)患者每年发生同侧乳腺导管癌(左)和浸润性癌(右)的风险
研究显示,在11337名患者中,有7204名(64%)患有高级别DCIS。随着时间的推移,高级别DCIS的比例升高(从60%到65%),低级别DCIS的比例减少(从10%到6%),肿瘤的平均大小增加(从21.4mm增加到24.1mm)。高级别DCIS(36%)患者的乳腺切除术相比于低等级DCIS(15%)更为常见。有很少一部分(6%)接受保乳手术(BCS)的患者的手术切缘<1mm。
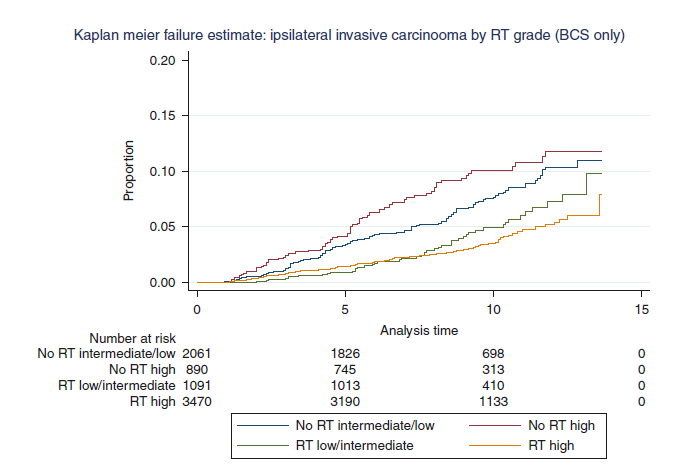
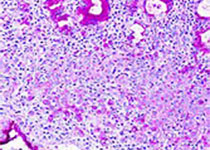
乳腺癌保乳手术患者放射治疗对同侧继发性浸润性癌的影响
在英格兰地区确诊的9191名妇女中(中位随访9.4年),有7%的患者发展为同侧乳腺DCIS或浸润性恶性肿瘤,而5%的患者发展为对侧乳腺DCIS或浸润性恶性肿瘤。最常见的同侧事件为浸润性癌(n = 413),中位时间62个月,其次是DCIS(n = 225),中位时间37个月。放疗(RT)对高级别DCIS的复发最具保护作用(接受RT的高级别DCIS患者的复发率为3.2%,而无RT治疗的高级别DCIS患者的复发率则为6.9%,而低/中级别DCIS分别为2.3%和3.0%)。进一步研究显示,同侧DCIS事件在5年后有所减轻,而同侧浸润性癌的风险一直会持续超过10年。
综上,该研究结果揭示,DCIS的病理学特征有助于患者管理,且强调对于DCIS患者需要进行长期的随访。
原始出处:
Shaaban, A.M., Hilton, B., Clements, K. et al. Pathological features of 11,337 patients with primary ductal carcinoma in situ (DCIS) and subsequent events: results from the UK Sloane Project. Br J Cancer (17 November 2020).
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#病理特征#
0
#CIS#
56
#原位癌#
86
#DCI#
42
#乳腺导管原位癌#
46