J Heart Lung Transplant:肺血管阻力指数预测肺动脉高压患者预后的性能优于肺血管阻力?
2021-05-10 Nebula MedSci原创
肺血管阻力指数预测肺动脉高压患者预后的性能优于肺血管阻力?
肺动脉高压(PAH)是肺高压(PH)的一种,其特征是小肺动脉进行性变窄,若不及时治疗,可导致右心衰竭和死亡。PAH的诊断需要独特的毛细血管前血流动力学特征,包括平均肺动脉压(mPAP)>20 mmHg、肺动脉楔压(PAWP)≤15 mmHg和肺血管阻力(PVR)≥3 Wood单位(WU)。
与肺血管阻力(PVR)相比,PVR指数(PVRI)解释了身体习性的变化。该研究测试了消瘦和肥胖(BMI≥30 kg/m2)的肺动脉高压患者的PVRI与PVR相比与临床预后的相关性。
这是一项回顾性研究,纳入了于1992年2月-2019年11月期间在Cleveland诊所进行了右心室导管检查的PAH患者。
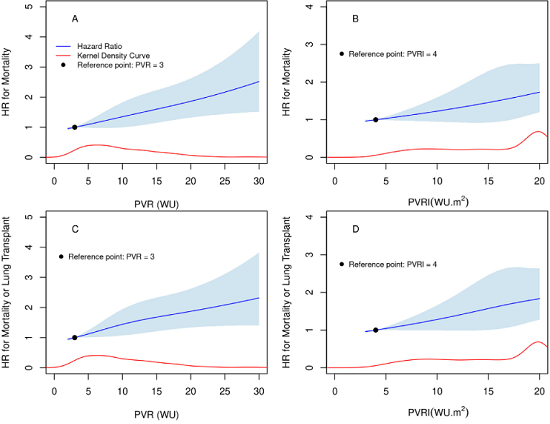
基于PVR和PVRI的死亡或肺移植风险
共涵盖了644位患者(平均 53±16岁,74%的女性)。特发性或遗传学PAH患者占所有患者的44%。随着体重的增加,心输出量增多(p<0.0001),而PVR降低了(p<0.0001)。
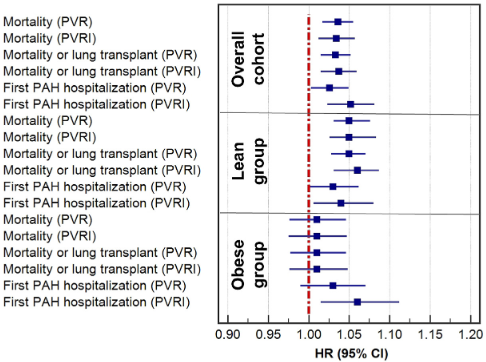
在整个队列、肥胖亚组和消瘦亚组中,基于PVR和PVRI的首次PAH住院、死亡或肺移植的风险比
PVR和PVRI均与疾病的严重程度相关,且与PVRI的关联更明显。在整个队列患者以及BMI<30 kg/m2的患者中,PVR和PVRI都是首次因PAH住院、死亡或肺移植的危险因素。
但是,PVRI还是肥胖患者首次因PAH住院的风险因素,但PVR不是。在肥胖患者亚组中,无论PVR还是PVRI都与死亡风险无关。
总之,该研究提示,PVRI似乎比PVR与PAH患者的疾病严重程度的相关性更强;但是,PVR和PVRI与整体队列受试者的住院和生存预后的相关性相似。
原始出处:
Khirfan Ghaleb,Li Manshi,Wang Xiaofeng et al. Is pulmonary vascular resistance index better than pulmonary vascular resistance in predicting outcomes in pulmonary arterial hypertension? J Heart Lung Transplant, 2021, undefined: undefined. https://doi.org/10.1016/j.healun.2021.03.022
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














#阻力指数#
36
#肺动脉高压患者#
37
#Transplant#
35
#患者预后#
37
#TRA#
27
#动脉高压#
27
#肺血管阻力#
43
#plant#
26
#ART#
30
#HEART#
25