NEJM:强大的交互工具ProteinPaint可深挖癌症基因组数据
2016-01-02 MedSci MedSci原创
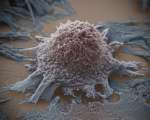
最近,来自圣犹大儿童研究医院的研究人员开发了一种新型的网络应用和数据装置,其就为全球科学家们提供了强大的交互工具帮助他们理解引发儿童癌症的各种突变,相关研究刊登于Nature Genetics杂志上。这种特殊的工具名为ProteinPaint,其可以帮助有效地揭示改变编码蛋白指令且引发儿童癌症的突变,该工具可为当前的工具提供关键的信息,比如其可以揭示突变是新诊断出的还是复发出现的,或者突变是否是在

最近,来自圣犹大儿童研究医院的研究人员开发了一种新型的网络应用和数据装置,其就为全球科学家们提供了强大的交互工具帮助他们理解引发儿童癌症的各种突变,相关研究刊登于Nature Genetics杂志上。这种特殊的工具名为ProteinPaint,其可以帮助有效地揭示改变编码蛋白指令且引发儿童癌症的突变,该工具可为当前的工具提供关键的信息,比如其可以揭示突变是新诊断出的还是复发出现的,或者突变是否是在所有细胞中发生或者仅是在癌症中发生的。
ProteinPaint工具的新型交互图谱可以帮助科学家们观察分析单一基因及编码的蛋白所发生的所有突变,其中就包括突变类型、癌症亚型的频率及蛋白结构域的位置,相关的信息或可帮助揭示癌症的起源、进展及复发的机制。Jinghui Zhang博士说道,新型工具对于帮助科学家们利用基因组数据进行癌症研究非常关键,而我们开发的ProteinPaint就可以帮助挖掘大量癌症基因组的数据以供科学家们进行研究。
目前存在多种类型的突变可以干扰编码蛋白的基因,以至于最终引发癌症,ProteinPaint工具可以整合来自多个数据装置中的突变信息,从而就增强了其功能,目前ProteinPaint工具中包含了在1000多名患21种类型癌症儿童中发现的几乎27500种突变的信息,而且这些数据也将会在近日进行更新。
该工具同时还可以对928名儿童中的36种癌症亚型肿瘤进行RNA序列数据的绘制,从而帮助追踪突变如何影响基因的表达,而与此同时进行全基因组测序就可以帮助揭示有机体的完整DNA组成;如今ProteinPaint工具重点对儿童癌症进行研究,其也具有帮助研究其它疾病的潜力,比如镰刀形细胞病等。最后研究者还补充道,该工具还会用于儿童癌症的种系突变研究,而相关研究也于近日刊登于国际杂志the New England Journal of Medicine上。
原始出处:
Jinghui Zhang, Ph.D., Michael F. Walsh, M.D., Gang Wu,et al. Germline Mutations in Predisposition Genes in Pediatric Cancer.N Engl J Med 2015; 373:2336-234 doi:10.1056/NEJMoa1508054
Zhou X, Edmonson MN, Wilkinson MR, Patel A, Wu G, Liu Y, Li Y, Zhang Z, Rusch MC, Parker M, Becksfort J, Downing JR, Zhang J. Exploring genomic alteration in pediatric cancer using ProteinPaint.Nat Genet. 2015 Dec 29;48(1):4-6.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#癌症基因#
29
值得进一步关注
106
是一篇不错的文章
107
这篇文章有一定深度
111
不错,赞一个
114
赞一个
102
赞一个
79
不错哦
76
有意思
136
#PRO#
20