JACC:无症状颅内动脉粥样硬化性狭窄的决定因素和预后
2021-08-07 Nebula MedSci原创
ICAS是无卒中病史受试者已明确的动脉粥样硬化疾病的影像学标志;一旦确诊ICAS后,应及时的对血管健康进行彻底的评估
颅内动脉粥样硬化狭窄(ICAS)是全世界最常见的卒中原因之一;即使对危险因素进行了积极的处理,但卒中复发的风险仍然很高。一项中国大规模多中心研究发现,46.6%中国急性缺血性脑卒中患者存在中度及以上ICAS,而一项基于社区的流行病学调查显示,在未发生过卒中和短暂性脑缺血发作人群中,13.6%的个体存在无症状性ICAS。
本研究旨在明确无症状颅内动脉粥样硬化狭窄患者的危险因素和血管事件风险的作用,以改进危险分层。
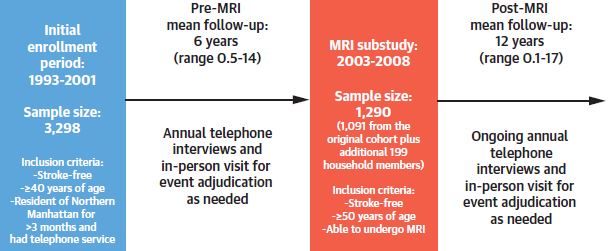
研究流程
在自1993年起进行的前瞻性NOMAS(北曼哈顿研究)试验中,随访的无卒中病史的参与者在2003年至2008年期间接受了脑磁共振血管造影。研究人员将11条脑动脉的狭窄程度划分为:0: 无狭窄;1: <0%或管腔不规则;2: 50%-69%;3: ≥70%狭窄或流隙,并评估了研究期间的血管事件发生情况。
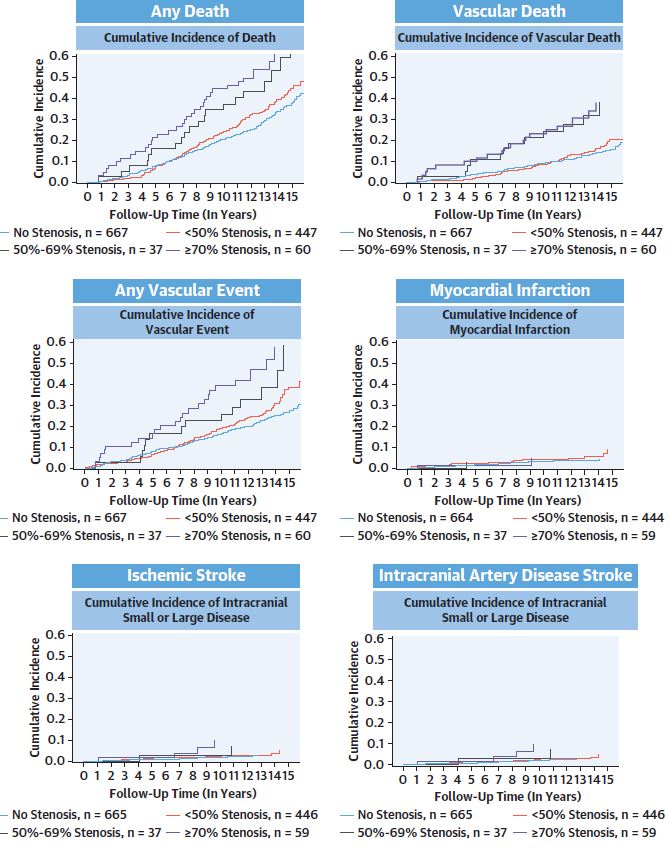
根据狭窄程度分层的各血管事件的累积发生率
总体上,共纳入了NOMAS试验的1211位参与者的样本(平均 71±9岁;59%的女性,65%的西班牙裔,45%的存在脑血管狭窄)。年龄越大(OR 1.02/岁)、高血压持续时间越久(OR 1.01/年)、降糖药物服用种类越多(OR 1.64/种)和高密度脂蛋白越低(OR 0.96/ mg/dL)与ICAS风险越高相关。ICAS≥70%的受试者的血管事件风险最高(血管事件的年风险 5.5%;与无ICAS的个体相比的风险比[HR] 2.1)。
简而言之,ICAS是无卒中病史受试者已明确的动脉粥样硬化疾病的影像学标志;一旦确诊ICAS后,应及时的对血管健康进行彻底的评估。
原始出处:
Jose Gutierrez, et al. Determinants and Outcomes of Asymptomatic Intracranial Atherosclerotic Stenosis. J Am Coll Cardiol. 2021 Aug, 78 (6) 562–571
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#JACC#
48
#决定因素#
46
#颅内动脉粥样硬化#
42
#粥样硬化性#
44
#粥样硬化#
34
很好
78
#ACC#
29
#无症状#
25
#硬化性#
40