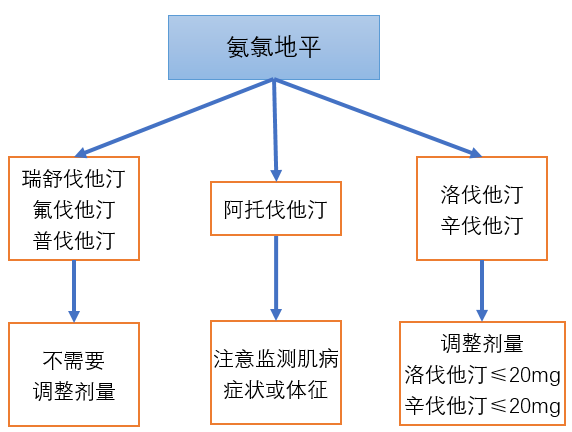
警惕:氨氯地平与这3种他汀的相互作用
2018-03-29 佚名 药品之声
在临床上,氨氯地平与他汀类药物合用非常广泛。许多医生和药师认为氨氯地平较安全,与他汀类降脂药不存在相互作用。但研究证明,氨氯地平与辛伐他汀和洛伐他汀合用时具有明显的相互作用,与阿托伐他汀合用时也可能会发生横纹肌溶解症。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












阿托伐他汀通过CYP3A4代谢,与CYP3A4强抑制药合用时,可引起阿托伐他汀的血药浓度升高。如红霉素、克拉霉素、伊曲康唑、HIV蛋白酶抑制剂(利托那韦、沙奎那韦等)等
46
#相互作用#
37
#氨氯地平#
43
#互作#
49
学习了.谢谢分享
82
这个资料好!收藏!
73
了解了解.继续关注
55
学习了.谢谢分享
73
学习了
76
学习了
30