在急性期植入颈动脉支架?或许还有更优的治疗方案!
2020-12-31 《门诊》杂志 门诊新视野
既往研究发现,在患者发生颈动脉狭窄的初期给予颈动脉支架会导致卒中和死亡风险升高。血栓保护措施一直是医师容易忽略的部分。数据显示,仅有不到50%的患者在接受CAS时采取了血栓保护措施。
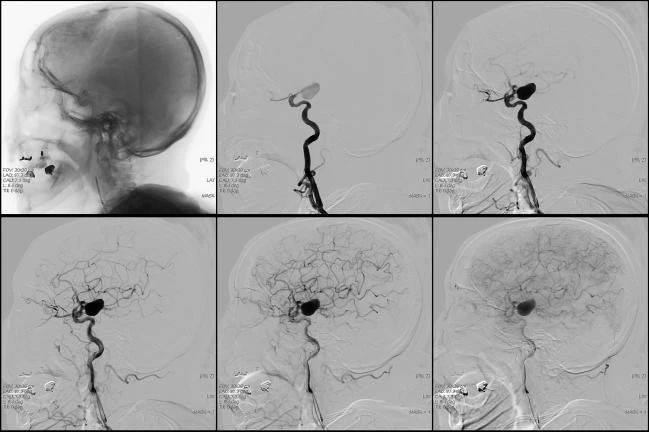
既往研究发现,在患者发生颈动脉狭窄的初期给予颈动脉支架(Carotid Artery Stenting, CAS)会导致卒中和死亡风险升高。最近,一项真实世界临床研究的数据进一步证实了这一研究结论。来自德国慕尼黑工业大学的Pavlos Tsantilas博士指出,基于目前的医学证据,我们发现,颈动脉内膜切除术(Carotid Endarterectomy, CEA)的临床效果优于颈动脉支架。这一结果是Tsantilas博士在研究了自2012年至2014年间德国共4717名症状性患者的数据后得出的。其他研究也发现,相比于CEA,当患者在症状发生的7天内接受CAS治疗时,其发生卒中或死亡的风险也会升高。来自美国纽约州布法罗大学的L. Nelson Hopkins博士指出,这一研究的局限性在于其忽略了血栓保护措施。血栓保护措施一直是医师容易忽略的部分。数据显示,仅有不到50%的患者在接受CAS时采取了血栓保护措施。
在研究中,数据显示,在神经性事件发生后两天内接受治疗的患者发生院内卒中或死亡的概率为6%,而在事件发生后3至7天接受治疗的患者发生院内卒中或死亡的概率为4.4%。然而,在第8至14天接受治疗和第15至180天接受治疗的患者中,院内卒中或死亡的发生率则分别为2.4%和3%。在调整分析中,较之那些在两天内就接受治疗的患者,在第8至14天接受治疗的患者发生院内卒中或死亡的风险更低(RR 0.47;95%CI 0.28-0.79),而且在第3至14天接受治疗的患者的全因死亡风险也较低。在这一研究中,入院接受治疗的绝大多数患者发生短暂性脑缺血发作(Transient ischaemic attack, TIA)或发生轻微卒中(Rankin 0-2)。
2016年发表的一项研究发现,当研究者利用CEA对同一数据库的患者进行治疗时,治疗的时间窗与患者发生卒中或死亡的风险并无太大关联。这一研究证实,在稳定性患者中,在患者出现神经性事件后可及早进行CEA以移除不稳定或易引发卒中的斑块。
在对四项临床研究(EVA-3S、SPACE、ICSS、CREST)进行综合分析后,研究者发现,在症状出现的前几周,相比于CEA治疗,CAS治疗将患者死亡或卒中的风险增加将近7倍。因此,研究者认为外科手术或许在急性期更为安全。然而另外一些研究者则认为,在这四项研究中,由于仅有CREST研究将血栓保护措施纳入方案,因此这一结果并不能很好地反映CAS的劣效性。此外,还有一些人认为早期CAS的经验不足可能也会导致较差的结果。
Tsantilas博士和他的研究团队称,无论是既往研究还是最新数据均表明,在神经系统事件发生的早期进行CAS治疗或许更危险。然而,Hopkins博士则提出了自己的看法:“我们无需关注过去的研究。随着医师经验越来越丰富,手术也会变得更加安全。”他认为“不支持医师使用颈动脉支架对患者进行治疗”缺乏一定的证据支持。他补充,在急性期时,血栓保护措施很关键。此外,近端血栓保护对于有引发卒中的斑块的患者大有裨益。
Tsantilas博士和他的研究团队建议对患者应首选进行外科手术治疗,相比于利用支架将斑块推向血管壁,利用远端或近端钳将不稳定的斑块移除更加安全。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














#颈动脉#
33
#急性期#
40
#颈动脉支架#
38
#治疗方案#
0
#植入#
33
好文章!
77