Blood:信号通路抑制剂在高危的慢性淋巴细胞白血病中的应用
2018-07-12 MedSci MedSci原创
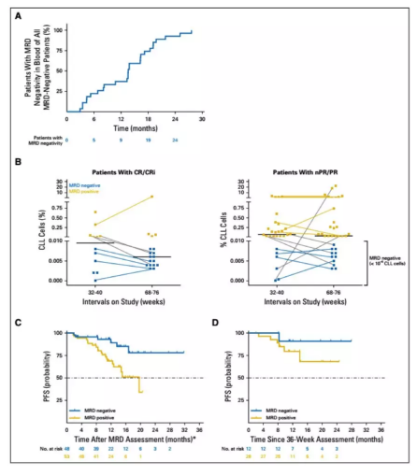
高风险的慢性淋巴细胞白血病(CLL)的定义是对化疗免疫疗法(CIT)具有临床和/或遗传抵抗(TP53异常)。随着通路抑制剂(PI)的可用性,如激酶抑制剂和BCL2拮抗剂,大大提高了CIT耐药性患者的预后。Peter Dreger等人建议修订高危型CLL的定义,即受TP53异常驱动、PI治疗可缓解。I型高危型CLL,CIT耐药的定义为携带TP53异常、临床上的CIT耐药性疾病,但PI治疗可完全缓解。
Peter Dreger等人建议修订高危型CLL的定义,即受TP53异常驱动、PI治疗可缓解。I型高危型CLL,CIT耐药的定义为携带TP53异常、临床上的CIT耐药性疾病,但PI治疗可完全缓解。这类疗法在很大程度上是以PI为基础的疗法的领域,而细胞疗法(如同种异体造血细胞移植)仍仅适用于部分相对风险低的患者。
II型高危型CLL,对CIT和PI耐药,其特点是药物治疗的可能性越来越小,这类患者可考虑采用细胞疗法(包括嵌合抗原受体编辑的T细胞)。此外,分子疗法和细胞疗法并不是相互排斥,或可联合应用探索其治疗潜能。
原始出处:
Peter Dreger,et al. High-risk chronic lymphocytic leukemia in the era of pathway inhibitors: Integrating molecular and cellular therapies. Blood 2018 :blood-2018-01-826008; doi: https://doi.org/10.1182/blood-2018-01-826008
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#淋巴细胞白血病#
30
#抑制剂#
32
学习并分享!!
72
#淋巴细胞#
36
#信号通路#
40