Cardiovasc Diabetol:过去40多年青少年的血压变化趋势
2022-01-04 Nebula MedSci原创
青少年血压升高与成年后高血压以及晚年时肾脏和心血管疾病的发病率和死亡率相关
在一般人群中,血压升高 (BP) 是导致心血管疾病发病率和死亡率升高的主要原因。目前,已有研究证明,青少年血压升高与成年后高血压以及晚年时肾脏和心血管疾病的发病率和死亡率相关,此外,还与早发糖尿病的风险增加密切相关。
大多数关于收缩压和舒张压趋势的数据都是基于对 10-20 年期间选定人群的调查。鉴于青少年肥胖率的持续升高,本研究旨在概述青少年人群血压的长期变化趋势。
这是一项全国性的基于人口的大规模研究,共纳入了 2,785,515 名以色列在 1977 年至 2020 年强制服兵役之前接受过医学评估并测量过体重、身高和血压的青少年(41.6%的女生,平均17.4岁)。研究期以 5 年为间隔。采用线性回归模型描述沿时间间隔趋势的 P 值。采用协方差分析计算根据体重指数调整的血压平均值。
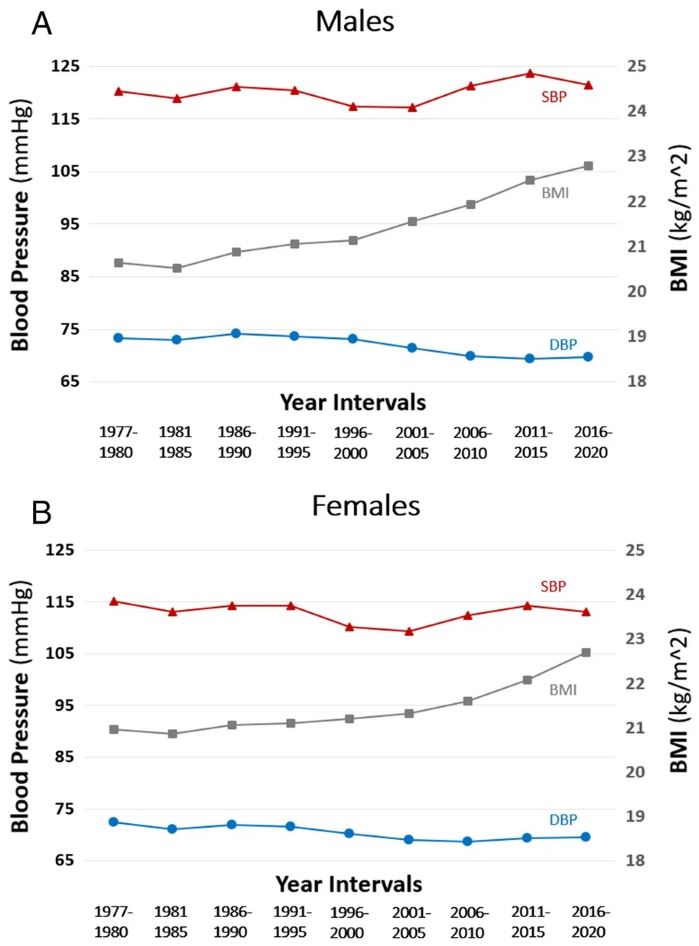
研究期间不同性别的青少年的血压的变化趋势
在研究期间,男生和女生的平均体重指数分别增加了 2.1 kg/m2 和 1.6 kg/m2(P 值均<0.001)。男生的平均舒张压降低了 3.6 mmHg,女生的平均降低了 2.9 mmHg(P 值均<0.001)。男生的平均收缩压升高了 1.6 mmHg,女生的平均降低了 1.9 mmHg。当根据体重指数调整血压值时,这些趋势保持不变。
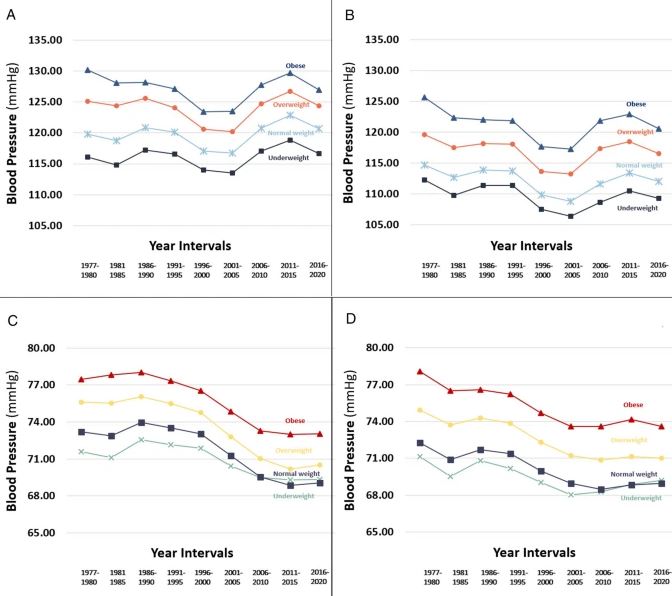
根据BMI调整的血压变化趋势
综上所述,尽管过去 40 年内以色列青少年的体重指数有所增加,但无论是男生还是女生,舒张压均有所降低;只有男生的收缩压略有升高,女生的则还是有所降低。
原始出处:
Fishman, B., Zloof, Y., Orr, O. et al. The opposing trends of body mass index and blood pressure during 1977–2020; nationwide registry of 2.8 million male and female adolescents. Cardiovasc Diabetol 20, 242 (2021). https://doi.org/10.1186/s12933-021-01433-0
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#BET#
33
#ASC#
36
#DIA#
35
#血压变化#
50