Nat Commun:钙离子通道蛋白发挥令人意想不到的作用
2017-03-30 生物谷 生物谷
2017年3月30日讯 /生物谷BIOON/ --近日,来自美国西北大学医学院的科学家们在国际学术期刊Nature Communicaitons上发表了一项新研究,揭示了钙离子释放激活钙离子通道(CRAC)家族的两个蛋白如何通过相互作用控制钙离子流入细胞,进而调节下游免疫应答。科学家们借助小鼠模型探索了ORAI1和ORAI2这两个CRAC通道蛋白如何控制CRAC通道活性和免疫应答。“目前大
近日,来自美国西北大学医学院的科学家们在国际学术期刊Nature Communicaitons上发表了一项新研究,揭示了钙离子释放激活钙离子通道(CRAC)家族的两个蛋白如何通过相互作用控制钙离子流入细胞,进而调节下游免疫应答。
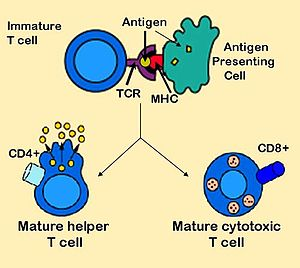
科学家们借助小鼠模型探索了ORAI1和ORAI2这两个CRAC通道蛋白如何控制CRAC通道活性和免疫应答。
“目前大部分研究都聚焦于ORAI1,我们对于ORAI1通道如何开启已经有了一个合理的认识,我们知道该分子特异性表达于免疫细胞,并且如果ORAI1发生失活突变将导致严重的免疫缺陷。同时还存在另外一个相关蛋白ORAI2,如果该分子被过表达也会影响CRAC通道的活性,但是直到现在,该蛋白在天然组织中的确切作用还没有得到完全了解。”文章作者Murali Prakriya教授这样说道。
在这项研究中,科学家们发现ORAI2能够减缓ORAI1引导钙离子的能力。如果将ORAI2蛋白从CRAC通道中去除,科学家们发现钙离子向细胞内的流入显著增加。
更进一步的研究还表明如果同时去除这两个蛋白会引起CRAC通道失去功能,导致T细胞功能受损。除此之外,虽然缺失了这两个蛋白的小鼠会出现免疫应答受损,但是小鼠也受到保护不会发生两种自身免疫疾病——大肠炎和移植物抗宿主疾病,这两种疾病都是由T细胞所介导。
文章作者表示他们的结果揭示了ORAI2如何通过与ORAI1相互作用调节钙离子流量,进而共同控制免疫应答,该研究为免疫相关疾病的治疗提供了新的潜在靶点。(生物谷Bioon.com)
本文系生物谷原创编译整理,欢迎转载!点击 获取授权 。更多资讯请下载生物谷APP.
原始出处:
Martin Vaeth et al. ORAI2 modulates store-operated calcium entry and T cell-mediated immunity, Nature Communications (2017). DOI: 10.1038/ncomms14714
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#COMMUN#
36
#离子通道蛋白#
41
#Nat#
43
#钙离子#
37
#离子通道#
48