JI:日本科学家开发人源化小鼠模型 在体研究NK细胞功能不再困难
2017-03-28 生物谷 生物谷
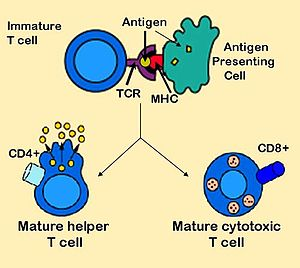
NK细胞是属于固有免疫系统的免疫细胞,在对抗侵入的病原体和微生物体方面发挥重要作用。NK细胞占循环系统中白细胞总数的大约5~20%,在癌症发育过程中也是执行“免疫监视”功能的重要细胞群体。NK细胞能够对肿瘤进行直接强力杀伤。目前科学家们借助NK细胞的这种杀伤能力开发了相应的癌症治疗方法。但是到目前为止关于人类NK细胞的研究还主要在体外进行,

NK细胞是属于固有免疫系统的免疫细胞,在对抗侵入的病原体和微生物体方面发挥重要作用。NK细胞占循环系统中白细胞总数的大约5~20%,在癌症发育过程中也是执行“免疫监视”功能的重要细胞群体。NK细胞能够对肿瘤进行直接强力杀伤。目前科学家们借助NK细胞的这种杀伤能力开发了相应的癌症治疗方法。
但是到目前为止关于人类NK细胞的研究还主要在体外进行,人类NK细胞在体内的功能还没有得到很好的了解。因此迫切需要用于研究NK细胞存活和长期维持的动物模型。
在这项研究中,来自日本庆应义塾大学的研究人员成功开发了一个人源化小鼠模型可以产生和维持人类NK细胞,用于细胞功能的体内研究。
在制备人源化小鼠模型的过程中研究人员构建了各种不同的小鼠品系,其中一种NOG-hIL-2小鼠可以表达人类细胞因子IL-2,可以支持T细胞的增殖。不幸的是,他们发现在移植了人类造血干细胞之后,小鼠体内产生大量人类NK细胞,除此之外,这些NK细胞还可以维持功能并在小鼠体内长期存活。
研究人员证实,不管在体内还是体外实验中这些NK细胞都能够强力抑制肿瘤生长。这一小鼠模型对于研究人类NK细胞在体内的生物学和病理学功能都有非常重要的价值。
原始出处:
Ikumi Katano et al. Predominant Development of Mature and Functional Human NK Cells in a Novel Human IL-2–Producing Transgenic NOG Mouse, The Journal of Immunology (2015). DOI: 10.4049/jimmunol.1401323
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#本科#
28
#日本#
30
#小鼠模型#
44
#细胞功能#
30
日本长期研究NK,终于有成果了
64