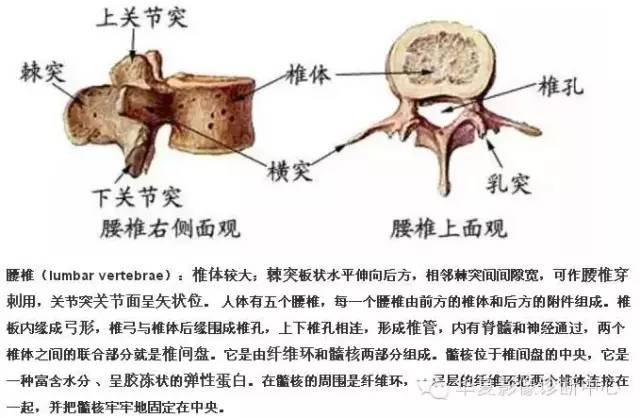
01 骶椎腰化/腰椎骶化 腰椎骶化及骶椎腰化均是椎骨发育的异常,腰椎骶化是指第五腰椎外型类似骶椎形态,并构成骶骨块的一部分,一侧或两侧横突肥大呈翼状,与骶骨发生融合或形成假关节。骶椎腰化是指第一骶椎演变成腰椎样形态,即第一骶骨从筋骨块中游离出来形成第6个腰椎。如何在临床阅片准确判断是一个很重要的问题,这里介绍一个最准确的判断方法。 这是一个最关键和准确的鉴定方法,国内著名骨放射学家杨世埙教授指导过,只要大家留意关注腰椎横突"三长/四翘/五宽",L3横突是最长的,L4横突是上翘的,L5横突最宽,特别用在胸椎腰化合并L5骶化的时候比较实用。 此外腰骶角的存在,对判断腰骶椎分界具有一定价值,不过存在水平骶椎是则较难做出正确判断。 下图为腰椎骶化 下图为骶椎腰化 02 椎体滑脱程度分级-Meyerding分级 Ⅰ度:椎体向前滑移程度不超过椎体中部矢状径的1/4。 Ⅱ度:椎体向前滑移程度超过椎体中部矢状径的1/4,但不超过2/4。 03 1.什么是腰肌劳损? 腰肌劳损是指因为腰背部肌肉、 筋膜、 韧带等软组织的慢性损伤,导致的局部无菌性炎症,从而引起腰背部一侧或两侧的弥漫性疼痛的临床综合征, 包括腰背肌筋膜炎、 肌纤维织炎、 肌筋膜疼痛综合征、 第三腰椎横突综合征 ,该病好发于 30 ~ 40 岁的青壮年男性,外伤及长期劳损为该病的主要发病诱因,此外还与气候、 空气湿度有很大的关系。 2.腰肌劳损的两大基础 解剖学:腰背部的结构肌肉主要包括腰背筋膜、 斜方肌、背阔肌、 骶棘肌、 横突棘肌( 半棘肌、 多裂肌和回旋肌) 和深层短肌( 横突间肌、 棘突间肌)。腰部是连接躯干和下肢的枢纽, 两侧的横突是腰肌和腰方肌的起点,并有腹横肌、 背阔肌的深部筋膜附着, 是腰部肌肉收缩运动的支点, 因此腰腹部肌肉弹力收缩时腰部受力最大, 且是躯干活动范围及强度最大的部位之一,易使肌肉及筋膜的附着点处形成无菌性的炎症,刺激局部的神经纤维,日久可以引起软组织变性,导致腰背部、 臀部及腿部疼痛。 病理学:长期不正确的姿势和负重, 使肌肉长期处于疲劳状态, 内外平衡失调, 力量不足, 使得韧带、 筋膜挫伤,肌肉纤维拉伤, 甚至出现局部的组织液渗出和微血管破裂, 蔓延到邻近肌间隙后形成瘢痕组织,最终导致局部粘连、 变性、 甚至肌肉萎缩,也就是肌筋膜炎,分布于肌肉组织中的神经纤维受到病变组织的压迫、 刺激甚至部分神经末梢被破坏,产疼痛感。 另一方面, 腰部软组织受到损伤之后未得到及时正确的治疗,或治疗不彻底, 或反复多次损伤, 致使受伤的组织不能完全修复, 局部存在慢性无菌性炎症,微循环障碍, 乳酸等代谢产物堆积, 加之受损的肌纤维变性或疤痕化, 也可刺激或压迫神经末梢而引起慢性腰痛 。两方面形成恶性循环, 使腰背部疼痛日益严重。 3.如何诊断腰肌劳损? 表现为反复发作的腰背酸痛、胀痛,偶有放射至下肢的疼痛感, 但通常不过膝 ,个别会有植物神经紊乱症状。在重体力劳动或活动后加重,并出现腰背部肌肉保护性僵直, 时轻时重,休息或改变姿势可缓解。压痛点不能精确定位, 但通常是位于腰椎横突、 骶棘肌及髂嵴后缘等部位,可以触诊到腰部肌肉的紧张,或有硬结及肥厚感,腰部外形及活动多无异常, 部分患者腰部活动稍受限。直腿高举试验阳性,也可以阴性, 但踝反射阴性,无伸拇肌力障碍。有部分患者的腰痛现象与气候及温度相关,比如阴冷、 潮湿的天气会引起或加重患者病情。 4.影像学表现 正常的肌肉在 MRI 上表现为形态饱满、 轮廓清晰平滑的均质低信号。男性的腰背肌厚度通常比女性要饱满,肌纤维也要粗大。 长时间的腰背部肌肉疲劳状态会导致其形态学发生改变,表现在肌肉体积的萎缩,肌肉边缘轮廓的模糊和凹陷,信号呈现出不均质改变, 这点在横轴位的脂肪压制像上体现得尤为明显。 从事体力劳动或体育活动的人群, 腰部肌肉尽管长时间处在疲劳当中,但是其从事的活动特殊性导致其肌肉纤维的增生和粗大, 腰部肌肉的萎缩和变性体现的不明显。 观察肌间隙的脂肪浸润也是衡量腰肌劳损的指标之一。脂肪浸润通常伴随有肌间隙的扩大,在MRI上呈现出三级信号 ,Ⅰ度表现为肌间隙显示不清或仅能显示线状、 点状间隙扩大; Ⅱ度显示为多灶性间隙扩大伴脂肪信号; Ⅲ度浸润表现为肌间隙呈羽毛状或网格状增宽,以上间隙的扩大和脂肪的浸润是相伴相生的,也就是说扩大的肌间隙里通常由脂肪填充。 腰肌劳损的特征性表现是肌筋膜炎。也就是位于肌间隙和肌骨间隙的组织液渗出, 组织粘连和积液,腰背部肌肉和筋膜的水肿信号是判断腰肌劳损的重要标志之一,且浅筋膜的病变发现率要高于深筋膜。具体表现为腰背部皮下、 腰肌及筋膜下线状、 条状或片状的长 T1长T2,FS-T2WI高信号。 配 图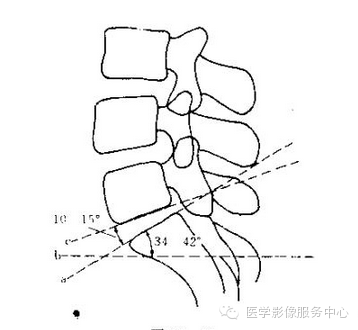




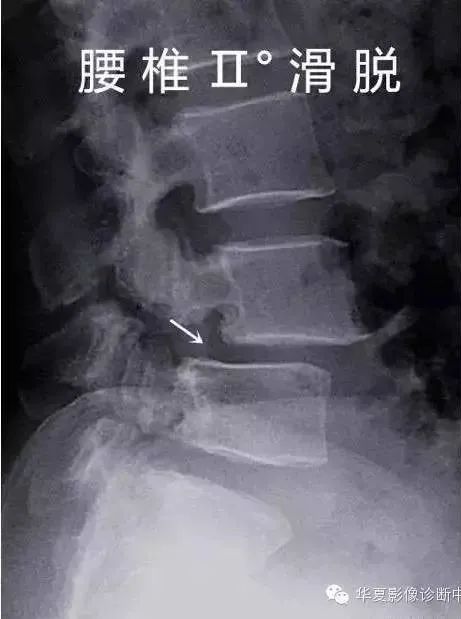
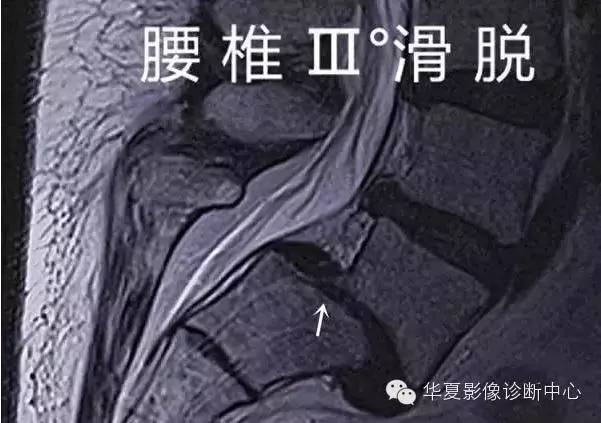
腰椎滑脱分度

Ⅲ度:椎体向前滑移程度超过椎体中部矢状径的2/4,但不超过3/4。
V度:椎体向前滑移程度超过椎体中部状径的3/4。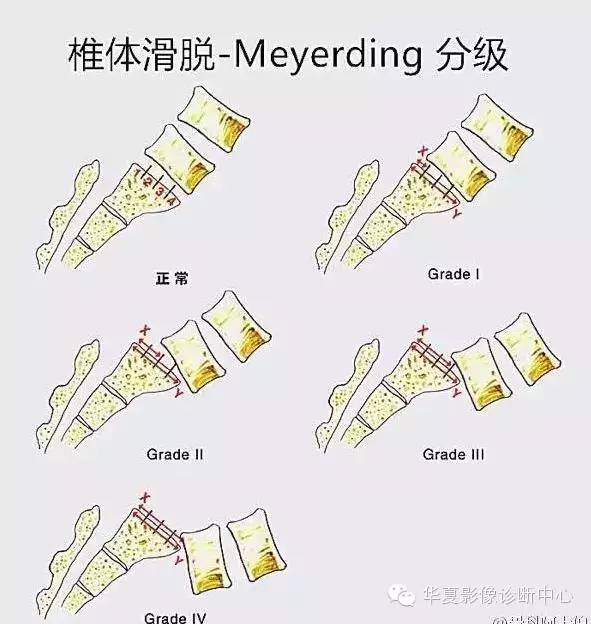



用磁共振看腰肌劳损


本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











学习了,非常棒
47
#腰椎骶化#
31
#腰椎#
36
真是好东西
70
好帖,学习
71
腰椎骶化及骶椎腰化均是椎骨发育的异
57
学习一下
68