Obstet Gynecol:美国年轻女性自我宫颈拭子采集检测HPV患病率分析
2016-11-25 haofan MedSci原创
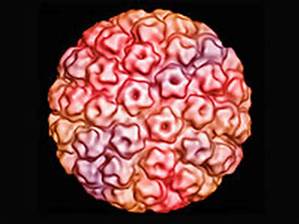
在美国HPV疫苗上市六年后,在接种一次或多次疫苗的妇女其与接种疫苗同一类型的HPV患病率有所下降,而与疫苗不属于同一类型HPV的患病率没有变化。此外,在未接种疫苗的妇女中,与HPV疫苗属于同一类型的患病率没有变化。
最近,妇产科领域权威杂志Obstetrics and Gynecology上发表了一篇研究文章,旨在评估在美国年轻女性中人类乳头状瘤病毒(HPV)患病率自HPV疫苗上市后在接种和未接种疫苗的妇女中有无发生变化。
研究人员针对这一问题进行了一项女性HPV患病率的回顾性调查,研究者通过国家健康和营养检查调查,对居住在美国年龄在18岁-29岁之间的女性进行分析,这个调查时个正在进行的一系列横断面调查。参与者需要对标准化的问题进行回答,并自我收集宫颈拭子标本,通过线性阵列HPV检测来确定HPV感染率。该研究在HPV疫苗上市以前(2003–2004年)对783名妇女和在HPV疫苗上市以后(2007–2012年)对1526名女性进行了分析。
研究人员发现在18岁–29岁的女性中,接种过一次或多次HPV疫苗的女性,与疫苗同一类型的HPV患病率明显降低(P=0.003):在疫苗上市前其该型HPV患病率为10.1%(95%可信区间为7.1–13.8%);在疫苗上市后,与接种疫苗同一类型的HPV患病率为4.2%(95%可信区间为3.3–10.9%)。然而,在接种一次或多次疫苗的妇女其与接种疫苗不属于同一类型的HPV患病率没有明显变化(P>0.05)。而且,在未进行疫苗接种的女性中,与疫苗同一类型的HPV患病率也无明显变化,在疫苗上市前为10.1%(95%可信区间为7.1–13.8%)疫苗上市后为8.8%(95%可信区间为5.6–12.9%)(P=0.4)。在2011年至2012年期间年龄为18-29岁的符合接种条件女性中接种疫苗的覆盖率增加至31.5%。
由此可见,在美国HPV疫苗上市六年后,在接种一次或多次疫苗的妇女其与接种疫苗同一类型的HPV患病率有所下降,而与疫苗不属于同一类型HPV的患病率没有变化。此外,在未接种疫苗的妇女中,与HPV疫苗属于同一类型的患病率没有变化。
原始出处:
Tarney, Christopher M, et al. Prevalence
of Human Papillomavirus in Self-Collected Cervicovaginal Swabs in Young Women
in the
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#NEC#
28
#检测HPV#
45
#TET#
26
辛苦编辑了,加油
65
#患病率#
31
#宫颈#
24
#年轻女性#
31
很好的研究,谢谢分享
55