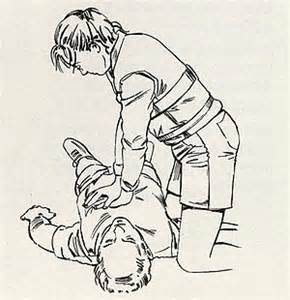
“抢救完手都在抖”高强度体力活的心肺复苏,来学吧
2017-06-22 山中麻署/复旦大学附属中山医院 澎湃新闻
曾经在逛知乎的时候看到过这样一个问题,“医生做心肺复苏累吗”?下面的十多个回答基本都是“非常累”、“喘成狗”、“抢救完手都在抖”、“汗滴都落在病人胸前了”之类的表示心肺复苏相当辛苦的答案。当然了,作为一个重症医学出身并且在麻醉科转基地的小麻花,小菌虽不是身经百战,但参与抢救做胸外按压的病例已经是两位数了。我这样没什么经验的年轻人,在抢救时主要是充当壮劳力,所以我充分了解持续高质量胸外按压是个非
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#心肺#
33
#复苏#
25
#抢救#
30
#高强度#
24
学习了
43
学习了,分享了
44