【所属科室】
内分泌科
【基本资料】
女,52岁
【主诉】
突发颈部肿物伴呼吸困难半日
【现病史】
患者发现甲状腺双叶多发肿物1年余,肿物逐渐增大,未予重视。昨晚无明显诱因肿物突然增大,位于颈部右侧,约5x5cm,质韧,光滑,与周围组织分界清,随吞咽上下活动。伴有压痛,伴轻度呼吸困难,无吞咽困难。
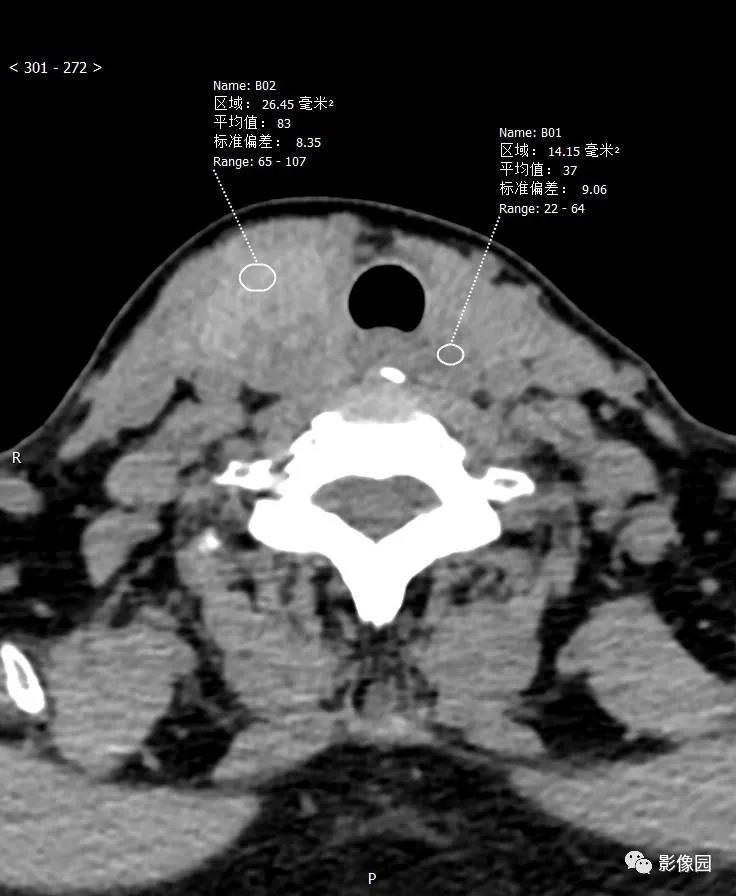
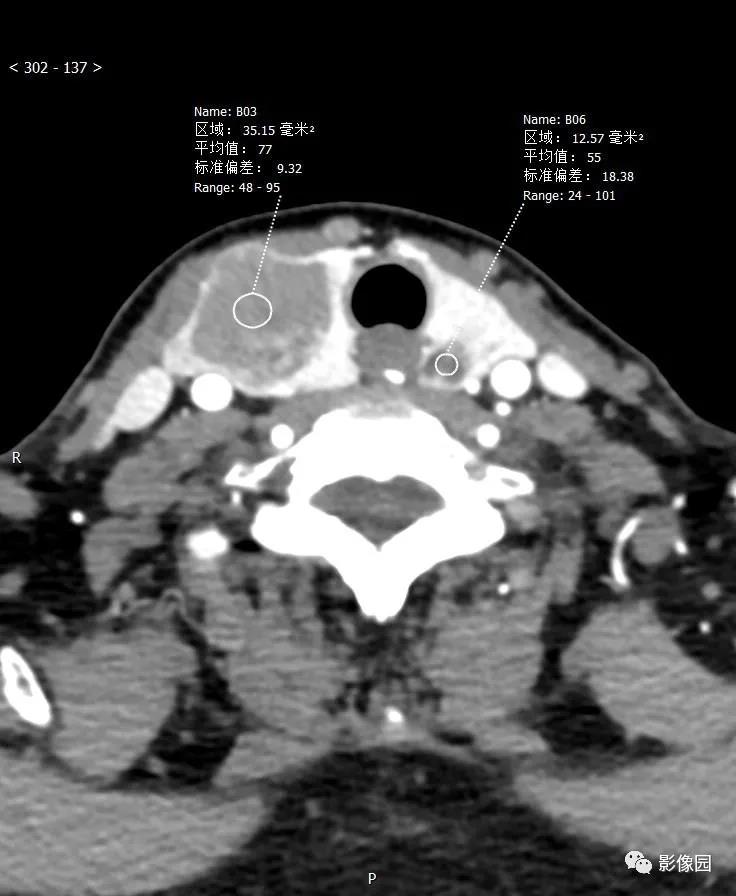
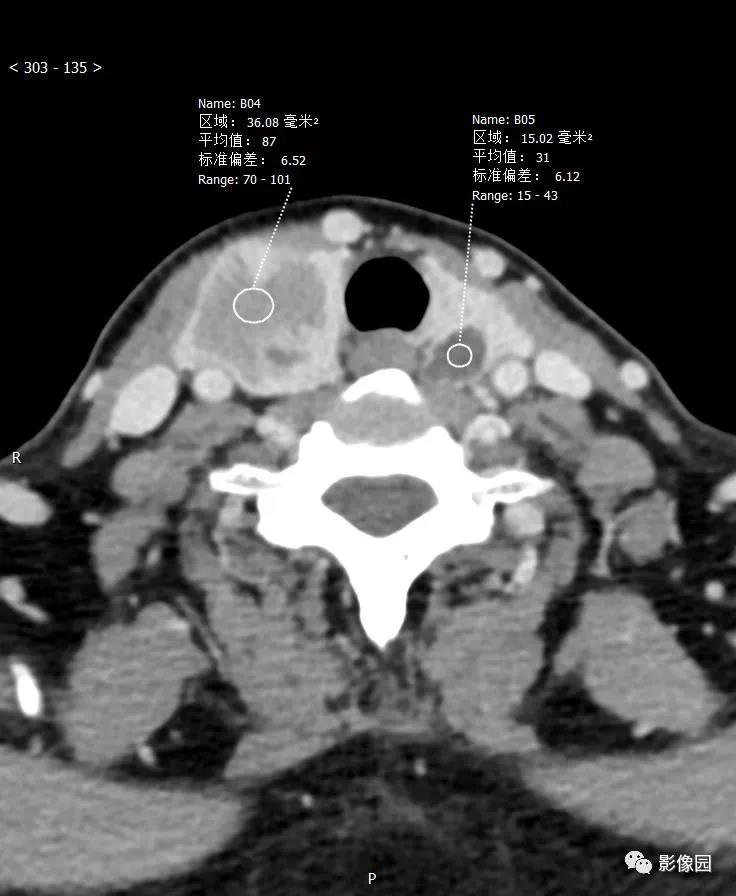
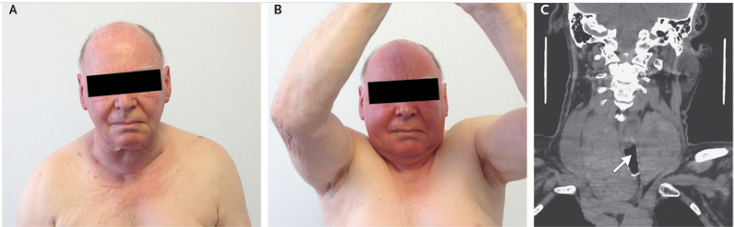
【影像图片】
【讨论问题】诊断?
【讨论】
评论:双侧甲状腺形态不对称,气管尚居中,右侧甲状腺体积增大,呈欠规则结节状稍高密度影,边界尚清。左侧甲状腺见小结节状稍低密度影,边界模糊。增强扫描右侧甲状腺病变未见强化,左侧甲状腺病变轻度强化。考虑:1)甲状腺肿;2)腺瘤
【结果】
(右侧甲状腺及肿物)结节性甲状腺肿伴出血、囊性变。
(左甲状腺)结节性甲状腺肿。
【病例小结】
甲状腺肿主要是由于缺碘引起的甲状腺代偿性增生,不伴由明显的甲状腺功能异常。初期甲状腺增大为弥漫性,可逐渐发展为结节状。
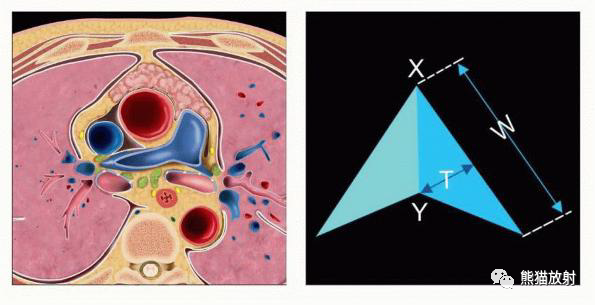
弥漫性甲状腺肿的病因可能是饮食中缺碘或甲状腺功能亢进或炎症。地方性甲状腺肿主要流行于碘缺乏区,女性居多,发病高峰为青春期。随时间推移,单纯性甲状腺肿可以发展为多结节性甲状腺肿,表现为甲状腺非对称性增大,可伸向胸骨后或上纵隔。75%~80%的胸骨后甲状腺肿起源于甲状腺下极或峡部。甲状腺内可见多发结节,并有局灶性出血、钙化、囊性变和瘢痕形成。
CT:单纯性甲状腺肿表现为甲状腺弥漫性肿大。甲状腺组织的CT值多在70HU以上。多结节性甲状腺肿则表现为甲状腺非对称性增大,伴有退行性变,出血、囊变、坏死或片状钙化则致密度不均。增强扫描,甲状腺组织增强,囊变坏死区不强化。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#肿物#
40
学习了
75
#呼吸困难#
48
#颈部#
34