Int Arch Allergy Immunol:过敏性鼻炎患者鼻黏膜细胞和血液中的不同的基因表达模式研究
2018-07-09 AlexYang MedSci原创
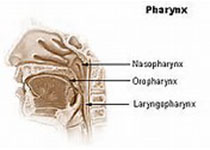
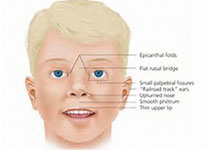
过敏性鼻炎(AR)基因表达的调查主要依赖于炎症部位的鼻活检样本或者血液样本(系统免疫)来获得用于分析的遗传材料。新的方法避免了侵入性样本搜集,并且为AR中相关的局部免疫机制更深入的了解提供了便利。研究人员在花粉高峰季节搜集了鼻洗液/鼻刷样本和全血样本比较分析了免疫基因的表达情况。研究包括了12名对花粉过敏的成年人(年龄46.3 ± 12.3岁),且患AR时间超过2年。研究发现,在不同的样本类型之间
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#过敏性#
30
#ALL#
25
#基因表达#
22
#黏膜#
22
v古古怪怪高好好干活
68
学习一下谢谢分享!
78
不错的文章值得推荐一下
75
不错的文章值得推荐一下
70
学习一下
69
学习了
19