Int Immunopharmacol:儿茶酸能够减轻过敏性鼻炎炎症
2018-06-29 AlexYang MedSci原创
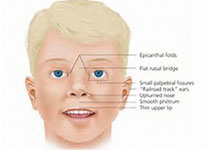
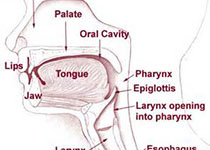
目前,过敏性鼻炎的流行度快速的增加。之前的工作阐释了儿茶酸的抗炎症作用,包括了过敏性疾病模型。然而,能够阐释该治疗作用的分子机制仍旧不清楚。胸腺基质淋巴细胞生成素(TSLP)来自于上皮细胞,已经被鉴定在过敏性疾病的发展过程中具有重要的作用,并且TSLP的产生与 NF-κB信号通路的激活相关。为此,有研究人员尝试研究了儿茶酸治疗过敏性鼻炎的情况,并且基于TSLP因子探究了所起作用的相关机制。研究发现
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#MAC#
30
#pharma#
36
#过敏性#
36
#Pharmacol#
27
#Pharm#
38
#茶#
27
学了
94
学了
84
不错
87
不错的文章值得拥有哦
91