JAHA:选择中高强度运动,预防痴呆更有效!尤其是男性
2021-01-24 “心关注”公众号 “心关注”公众号
在老龄化社会不断加剧的今天,痴呆症在全球范围内的发病率与患病率一直高居不下,目前仍呈逐年上升的趋势。
在老龄化社会不断加剧的今天,痴呆症在全球范围内的发病率与患病率一直高居不下,目前仍呈逐年上升的趋势。
世界卫生组织曾表示,对于 60 岁及以上的成人,痴呆症所造成的伤残调整寿命年(DALY)高于卒中、心血管疾病、癌症等。
一、世界范围内的痴呆症患病率
伦敦大学国王学院精神病学研究所 Martin Prince 研究团队 2013 年发表在《Alzheimers & Dementia》杂志上的系统评价与meta分析有统计,2010 年,全球约有 0.356 亿痴呆症患者,2030 年预计将涨幅 85%,达到 0.657 亿,到 2050 年甚至可能会上升到 1.154 亿。
东亚地区国家痴呆症的患病率相对较低,但未来的涨幅却很可能高于世界平均水平。下图较详细地展示了世界范围内各地区痴呆症的患病率,以及 2030 年、2050 年的预期涨幅。
二、AD发病前的病理生理变化
现有证据表明,在痴呆症临床症状出现前的数十年,人体就已经开始出现神经病理上的改变。
美国华盛顿大学医学院神内科 Randall J Bateman 研究团队既往发表在四大医学期刊之首《The New England Journal of Medicine》杂志上的前瞻性纵向临床研究中,检查评估了 128 例受试者的认知功能、脑影像学、脑脊液等,并统计了 88 例常染色显性阿尔梅茨海默病受试者父母的发病年龄,来推断受试者距发病的预期剩余年限。
研究发现,在常染色体显性遗传阿尔梅茨海默病发病前 10-25 年,就开始逐渐出现脑脊液中 Aβ42(下降)、tau 蛋白(上升)等指标的变化,以及脑体积萎缩、锲前叶葡萄糖代谢减低等病理生理变化。致病基因携带者(红线)与非携带者(蓝线)的各项指标,随时间发展的走势变化见上图。
三、痴呆与心血管疾病的共同危险因素
越来越多的研究证据证实,久坐、体力活动不足、脂质/葡萄糖代谢紊乱、高血压等,既是心血管疾病的危险因素,也是认知衰退与痴呆的风险因素。
比如美国梅奥诊所 D Knopman 研究团队既往发表在《Neurology》上的研究,以动脉粥样硬化性心血管疾病的多个危险因素进行分层,使用词语延迟回忆测试(DWR)、数字符号替换测试(DSS)及语言流畅测试(WF)等,评估各分层人群的认知功能。结果发现高血压、高血脂、糖尿病等同样是认知衰退的危险因素,具体数据见下表:
四、预防延缓痴呆症,推荐运动策略
预防痴呆症,或推延痴呆症的发病年龄,将有效延长患者的预期寿命,降低致残率,减少医疗保健费用的支出,并提升生活质量。现阶段用于治疗痴呆症的可用药物有限,且往往只能改善患者症状,目前急需制定合适的行为策略来预防推延痴呆症的发生,或延缓痴呆症的病程发展。
为了进一步推进这一领域的探索,美国老年国家研究所 2016 年发布了老龄化研究指导策略,强调了影响中老年人健康衰老过程中的行为、社会、心理和经济等因素。
增加中等至高强度的体育活动(MVPA),被认为是一种有望降低痴呆症发生风险和保护认知功能的有效策略。2018 年,美国体力活动指南委员会在分析现存文献研究的基础上,在指南更新中提出,MVPA 与大脑健康的关联性较强,包括大脑的信息处理速度、记忆力、认知功能、执行功能等,以及降低痴呆症的发生风险。
然而,既往发表在《American Journal of Preventive Medicine》杂志上的研究统计中,分析了美国国家健康与营养调查(NHANS)中的数据,结果发现:能够达到 MVPA、M2VPA 或 METPA 运动标准的居民,占比分别仅有 8.2%、9.6%、44.6%,均在 50% 以下。
在进一步分层后发现,不同性别、年龄、种族及受教育程度人群中,运动情况也存在较大差别。下图提供了对总人群进行各类分层后的详细数据:
基于完成中等至高强度的体育活动(MVPA)策略的人群比例较低,对于相当一部分成人群体,尤其是对于广大身体运动条件较差且认知功能下降风险较高的中老年人来说,是否可以提供一种替代策略,比如增加轻强度体力活动(LPA)来减少久坐行为,会不会更合适。
五、JAHA最新研究
既往研究更多的是分析中等至高强度的体育活动(MVPA),尚没有结合久坐行为(SED)、轻强度体力活动(LPA),来进一步关联认知功能的研究。
美国爱荷华大学 Kara M. Whitaker 研究团队假定每天用 LPA 或 MVPA 替代 30 分钟的久坐,5 年、10 年后的认知功能会相对更好,并于 2021 年 1 月 20 日将研究结果发表在了《Journal of the American Heart Association》杂志上。
该研究从青年人冠状动脉危险因素研究(CARDIA)中纳入了 1970 例符合标准的患者,这些患者在 2005-2006 年间佩戴可判断运动状况的加速度传感器,并在 5 年和/或 10 年后使用数字符号替换测试(DSST)、雷氏听觉词语学习测试(RAVLT)、斯特鲁普测试(Stroop)评估了患者的认知功能。
研究发现,在男性患者中:
DSST 评估结果:每天用 30 分钟 MVPA 替代 30 分钟 LPA 的组别,DSST 评分更优;而每天用 30 分钟 LPA 替代 30 分钟久坐的组别,DSST 评分更差。
RAVLT 评估结果:每天用 30 分钟 MVPA 替代 30 分钟 LPA 的组别,以及每天用 30 分钟 MVPA 替代 30 分钟久坐的组别,RAVLT评分更优;而每天用 30 分钟 LPA 替代 30 分钟久坐的组别,RAVLT 评分却更差。
Stroop 评估结果:每天用 30 分钟 MVPA 替代 30 分钟 LPA 的组别,Stroop 评分更优;而每天用 30 分钟 LPA 替代 30 分钟久坐的组别,Stroop 评分更差。以上较差的评估结果,可能与研究设计不足所带来的系统误差相关。
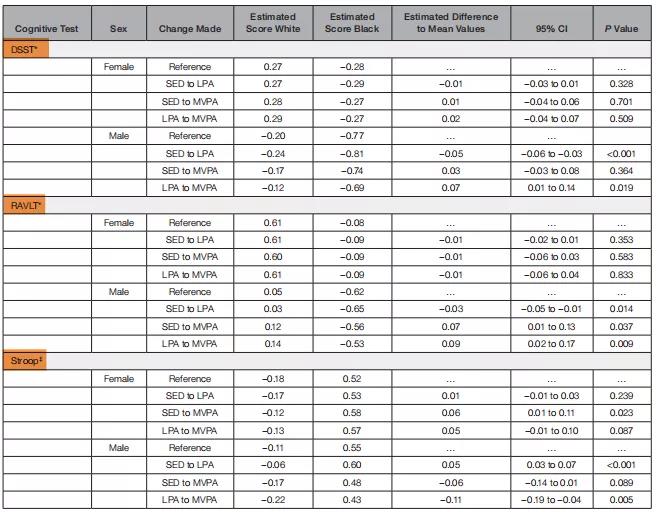
而在女性患者中,仅在 Stroop 评估结果中,每天用 30 分钟 MVPA 替代 30 分钟久坐的组别,结果更差;其余认知评估结果,均无显着差异。可能原因包括:与男性相比,女性的认知功能基线相对较高,或女性的实际运动强度相对较低等等。
六、研究结论
研究建议,中年男性应坚持中高强度的运动,以降低未来认知功能下降的风险。
未来应优化研究设计,同时检测患者的影像学及其他相关指标,并进一步观察分析性别差异。
原始出处:
Whitaker KM, Zhang D, et al. Longitudinal Associations of Midlife Accelerometer Determined Sedentary Behavior and Physical Activity With Cognitive Function:The CARDIA Study. Journal of the American Heart Association. (Published: 20 Jan 2021)
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#预防痴呆#
28
#AHA#
21
#高强度#
35
good for theword
72
好文章
71
#痴呆#
235
老年人痴呆何药可用??
45
666
74