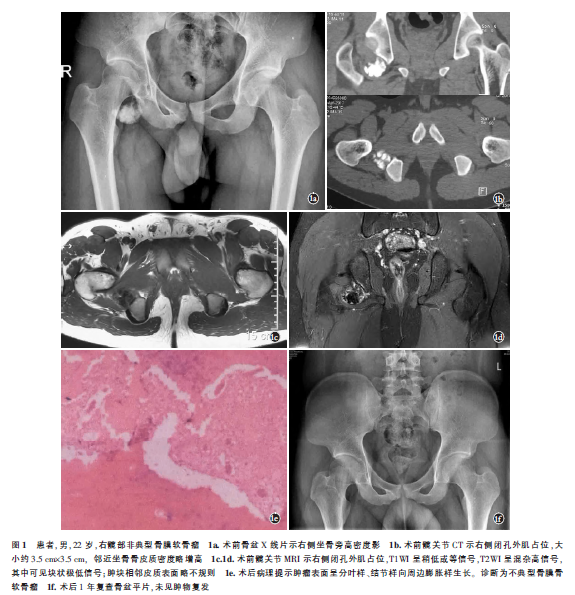
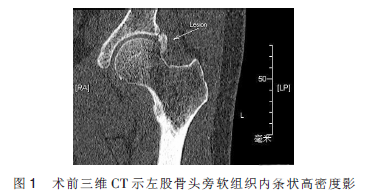
髋部非典型骨膜软骨瘤1例
2018-10-23 杨勇志 刘凡 张德宝 中国骨伤
患者,男,22岁,入院前7个月无明显诱因出现右侧髋部疼痛,行走时加重,休息可缓解。无发热、盗汗及夜间痛,无外伤史。前往当地医院拍片未见异常,未予处理。近40d来症状加重,并伴右侧髋部活动受限,遂来我院就诊。查体:右侧髋部无红肿,右侧腹股沟中点及右侧坐骨内侧压痛阳性,右髋后伸、外展受限。右髋Tomas征阳性,“4”字试验阳性。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












学习
61
#髋部#
26
#非典型#
31
#软骨瘤#
41
学习了
68