J Thromb Haemost:上肢深静脉血栓的抗凝治疗
2021-12-08 MedSci原创 MedSci原创
在上肢深静脉血栓形成患者中,抗凝治疗与较低的VTE复发风险和不容忽视的大出血风险相关。
上肢深静脉血栓形成的抗凝治疗数据主要来自对常见部位静脉血栓栓塞(VTE)的研究。

近日,血栓和凝血疾病权威杂志Journal of Thrombosis and Haemostasis上发表了一篇研究文章,该荟萃分析的目的是评估抗凝治疗对上肢深静脉血栓形成的有效性和安全性。
研究人员检索了MEDLINE和EMBASE数据库,纳入了包含上肢深静脉血栓形成患者的研究。该荟萃分析的主要结局是复发性VTE和大出血,次要结局包括临床相关的非大出血和全因死亡率。研究人员通过随机效应荟萃分析计算了包含95%置信区间(CI)的汇总估计值。
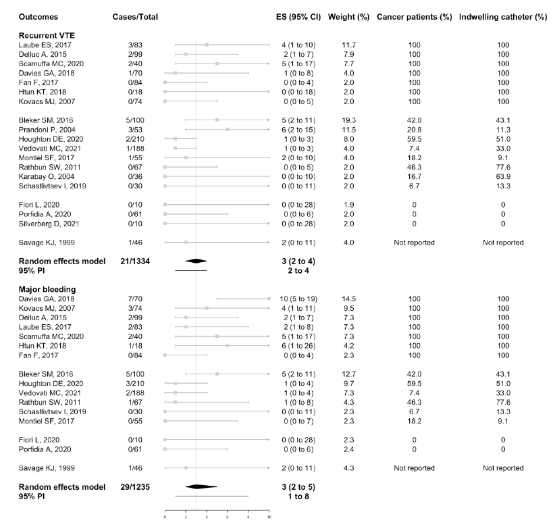
该研究共纳入了11项前瞻性研究和9项回顾性研究,共计1473名患者。60%的患者伴有留置导管,56.1%的患者患有癌症。分别有45.1%、35.0%和19.9%的患者接受了直接口服抗凝剂、低分子肝素和维生素K拮抗剂进行抗凝治疗,以及单独使用低分子肝素治疗。在13个月的中位随访期间,3%的患者(95%CI为2%至4%;21/1334名患者)发生了VTE复发,3%(95%CI为2%至5%;29/1235名患者)发生大出血,临床相关的非大出血为4%(95%CI为3%至6%;40/1075名患者),全因死亡率为9%(95%CI为5%至15%;108/1084名患者)。这些结果的发生率在伴有或不伴有癌症的患者、伴有或不伴有留置导管的患者以及接受不同抗凝治疗的患者之间没有显著差异。
由此可见,在上肢深静脉血栓形成患者中,抗凝治疗与较低的VTE复发风险和不容忽视的大出血风险相关。
原始出处:
Emanuele Valeriani.et al.Anticoagulant treatment for Upper Extremity Deep Vein thrombosis: a systematic review and meta-analysis.Journal of Thrombosis and Haemostasis.2021.https://onlinelibrary.wiley.com/doi/epdf/10.1111/jth.15614
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#静脉#
33
#静脉血#
32
#HAE#
38
学习了
48
学习了
67