Sci Rep:自我报道的过敏性鼻炎中敏感模式和过敏原最小筛选组合
2017-09-07 AlexYang MedSci原创
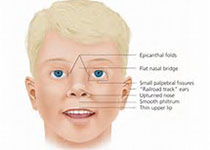
皮刺试验(SPT)组合的优化,尤其是不同地区具有不同敏感性模式显著差异时,在中国显得很有必要。最近,有研究人员进行了旨在评估过敏性鼻炎(AR)中过敏原敏感性的模式和临床相关性,并且确定了SPT过敏原最小组合,并通过K?ppen-Geiger气候地图进行分类。研究总共包含了7148名自我报道AR的受试者,他们完成了一份标准的调查问卷,并且通过SPT来进行相关过敏原敏感性评估。研究发现,6340(88
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#过敏性#
34
#自我报道#
34
我学习了.感谢分享
61
#过敏原#
28
#筛选#
0
学习了.涨知识了!
52