INVEST RADIO:影像学角度评估DCE-MRI中造影剂的浓度
2022-07-14 shaosai MedSci原创
动态对比增强磁共振成像(DCE-MRI)获取一系列多期相图像以监测GBCA在感兴趣的显影情况,这也可以通过对比剂动的力学参数来定量测量。
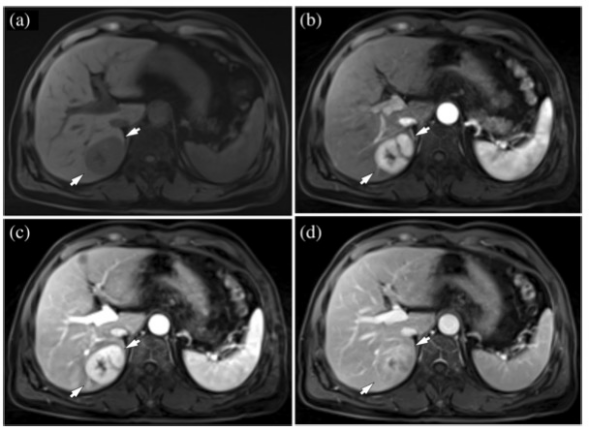
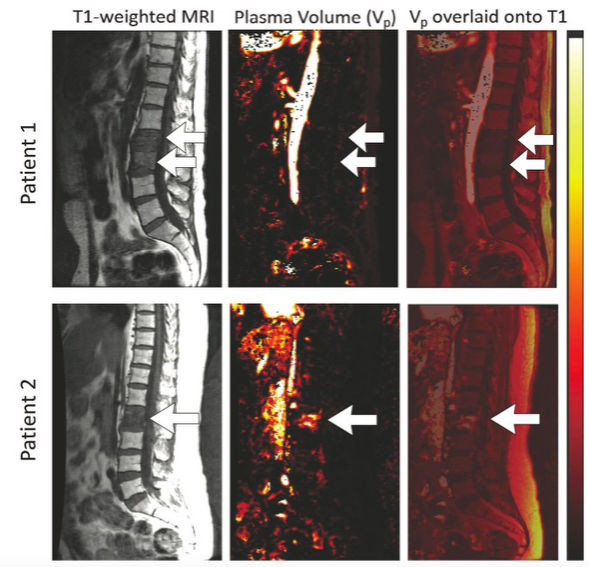
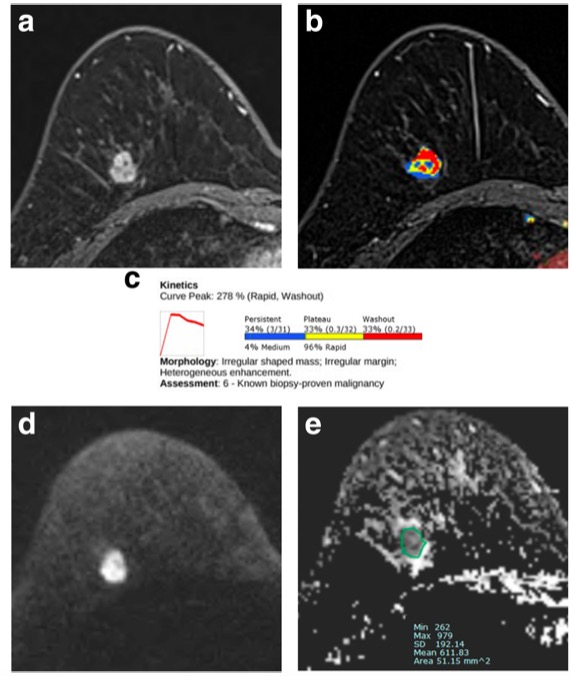
钆造影剂(GBCA)是细胞外造影剂,常用于临床的多部位影像学成像。 动态对比增强磁共振成像(DCE-MRI)获取一系列多期相图像以监测GBCA在感兴趣的显影情况,这也可以通过对比剂动的力学参数来定量测量。这些参数包括血浆流量(Fp)、血管渗透性表面积(PS)、血管血浆体积分数(vp)和血管外细胞体积分数(ve),是组织微循环环境的特异性参数,可用于癌症的诊断以及预测和监测治疗反应。
最近,Huang等专家研究了9个独立部位的动脉输入函数(AIF)测定的变化对前列腺癌DCE-MRI数据的药代动力学分析的影响,并报道了AIF振幅和形状的巨大变化是导致估计的药代动力学参数的主要因素之一。
近日,发表在INVEST RADIO杂志的一项研究在超短回波时间(UTE)的DCE-MRI扫描中使用2个翻转角(FAs)来同时评估强化前T1,并进一步准确评估GBCA浓度,为临床提供了一项影像学评估GBCA药代动力学及肿瘤治疗效果的新思路。

本研究应用C57BL/6J小鼠进行了T1加权DCE-MRI的3个连续的2个FAs扫描方案。在将时间-强度曲线转换为时间-浓度曲线的过程中,2个FA的数据被用来评估T10(T1T)。使用三种剂量的钆造影剂以达到在注射后10分钟测量钆浓度时的广泛变化范围:0.05 mmol/kg(n = 6)、0.1 mmol/kg(n = 11)和0.15 mmol/kg(n = 7)。使用强化前扫描测得的T10(T1M)以及文献中的恒定T10(2.1秒)(T1C)进行了信号到浓度的转换。利用DCE-MRI数据估算的采血时间钆浓度([Gd]T1T、[Gd]T1M和[Gd]T1C,分别)与电感耦合等离子体质谱法([Gd]MS)测量的血样的[Gd]进行了比较。此外,对患有GL261脑瘤的小鼠(n = 5)使用3种不同的方法进行了T10的对比动力学模型分析。
本研究表明,T1T与T1M强烈相关(r = 0.81),[Gd]T1M和[Gd]T1T与[Gd]T1C有明显不同,[Gd]T1M和[Gd]T1T与[Gd]MS有很好的一致性,其强相关性(平均百分比误差±标准差)分别为r=0.70(16%±56%)和r=0.85(15%±44%)。相比之下,[Gd]T1C的相关性较弱,为r = 0.52,误差较大,为33%±24%。使用T1T的GL261脑瘤的造影剂动力学模型参数与使用T1M的参数没有明显差异。

图 动脉输入功能的血管体素选择是基于曲线下的初始面积(IAUC)。A, DCE-MR图像在基线(30秒)、增强峰值(75秒)、高FA(300秒)和廓清结束(610秒)的代表性三维MIP渲染,红点表示所选10个血管的位置。B,在AIF增强峰值的三维图像的轴位图像上的AIF10个选定的血管像素(红色)显示
本研究使用2个FA进行了DCE-MRI研究,证明(1)用1个以上的FA获得的动态数据可以用来估计增强前的T1值,且不需要使用额外的扫描时间来单独测量T10;(2)使用强化前T1值估计的[Gd]与ICP-MS的测量结果接近,这是测量Gd的标准规范。因此,从改进的Gd定量中优化的药代动力学参数将使DCE-MRI成为临床上更有力的影像学工具。
原文出处:
Ayesha Bharadwaj Das,James Andrew Tranos,Jin Zhang,et al.Estimation of Contrast Agent Concentration in DCE-MRI Using 2 Flip Angles.DOI:10.1097/RLI.0000000000000845
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#EST#
43
#DCE-MRI#
49
#造影#
49
#浓度#
49