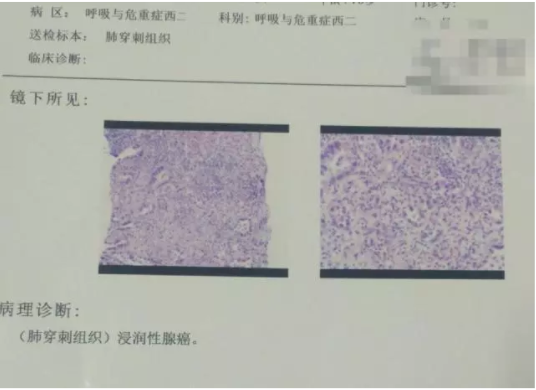
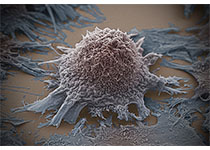
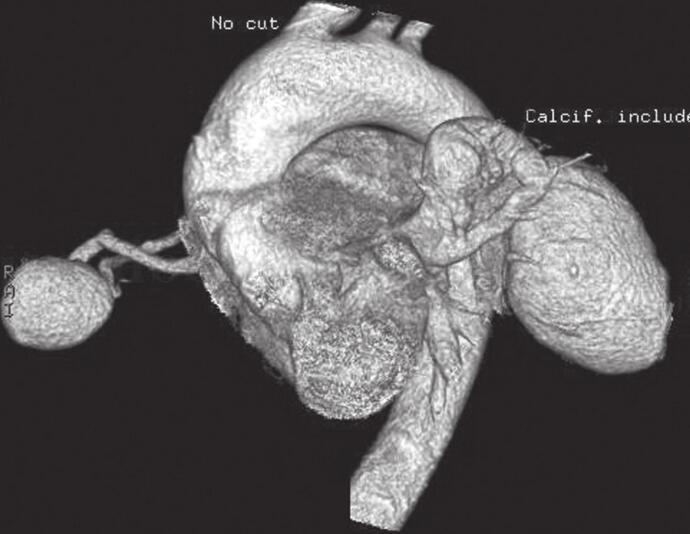
病例分享:面对越来越多的肺小结节应该怎么办?什么方法能解决肺小结节有恶性倾向又不适宜手术的难题?
2018-04-02 王瑞、范晓云 呼吸界
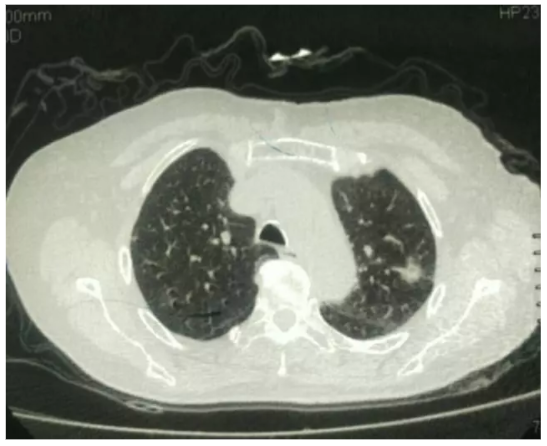
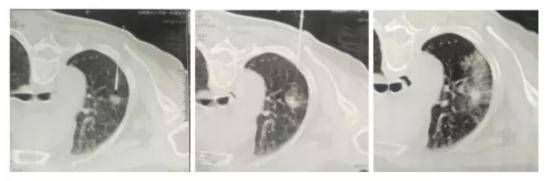
随着低剂量螺旋CT的逐渐普及,越来越多的人在体检中发现肺部结节,或者在治疗其他肺部疾病时发现肺部结节,随之而来的十分令人困扰的问题就是:这些结节是良性还是恶性?该如何处理?该不该手术?如果选择定期随访,会不会在随访过程中病灶增大等等……

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








很好的一个学习范例
63
#小结节#
25
学习了
69
学习学习
65
好
62