Dig Dis Sci: 合生元在中重度和重度急性胰腺炎中可以减少全身炎症反应和脓毒性并发症的风险
2022-07-31 xuyihan MedSci原创
急性胰腺炎是内科的一种急腹症,因为各种原因引起的胰腺激活作用,在胰腺组织后产生炎症反应。一般可伴有或者不伴有其他器官的并发症或者功能改变。
急性胰腺炎具有不同且不可预测的疾病进展,比如从良性的预后到暴发性炎症表现,最终会导致系统性炎症反应综合征 (SIRS) 和多器官功能障碍的出现。因此,治疗方式应侧重于减少炎症过程的程度并预防器官损伤和败血症的发生。肠道屏障在急性炎症中受损,会导致“细菌易位”,被认为是导致败血症的主要诱因。考虑到保护肠黏膜的重要性,临床上采用了各种治疗方式,如早期肠内营养和积极的静脉补液,用于预防肠道屏障功能衰竭。合生元通过维持肠道完整性和预防细菌易位在减少脓毒症并发症中的作用被认为是减少感染的潜在干预措施。本研究旨在评估合生元在减少中重度和重度急性胰腺炎脓毒症并发症方面的功效。
这是一项前瞻性随机对照研究。所有中重度和重度急性胰腺炎患者均纳入研究。研究人员将患有急性慢性胰腺炎、外伤性胰腺炎、ERCP和恶性肿瘤的患者排除在外。每天两次给患者服用1克含有益生菌的合生元,持续14天,对照组服用外观相似的安慰剂。并对患者进行了90天的随访。主要观察结果是减少脓毒症并发症和炎症标志物水平。次要观察结局是死亡率、非脓毒症发病率、住院时间 (LOH) 。

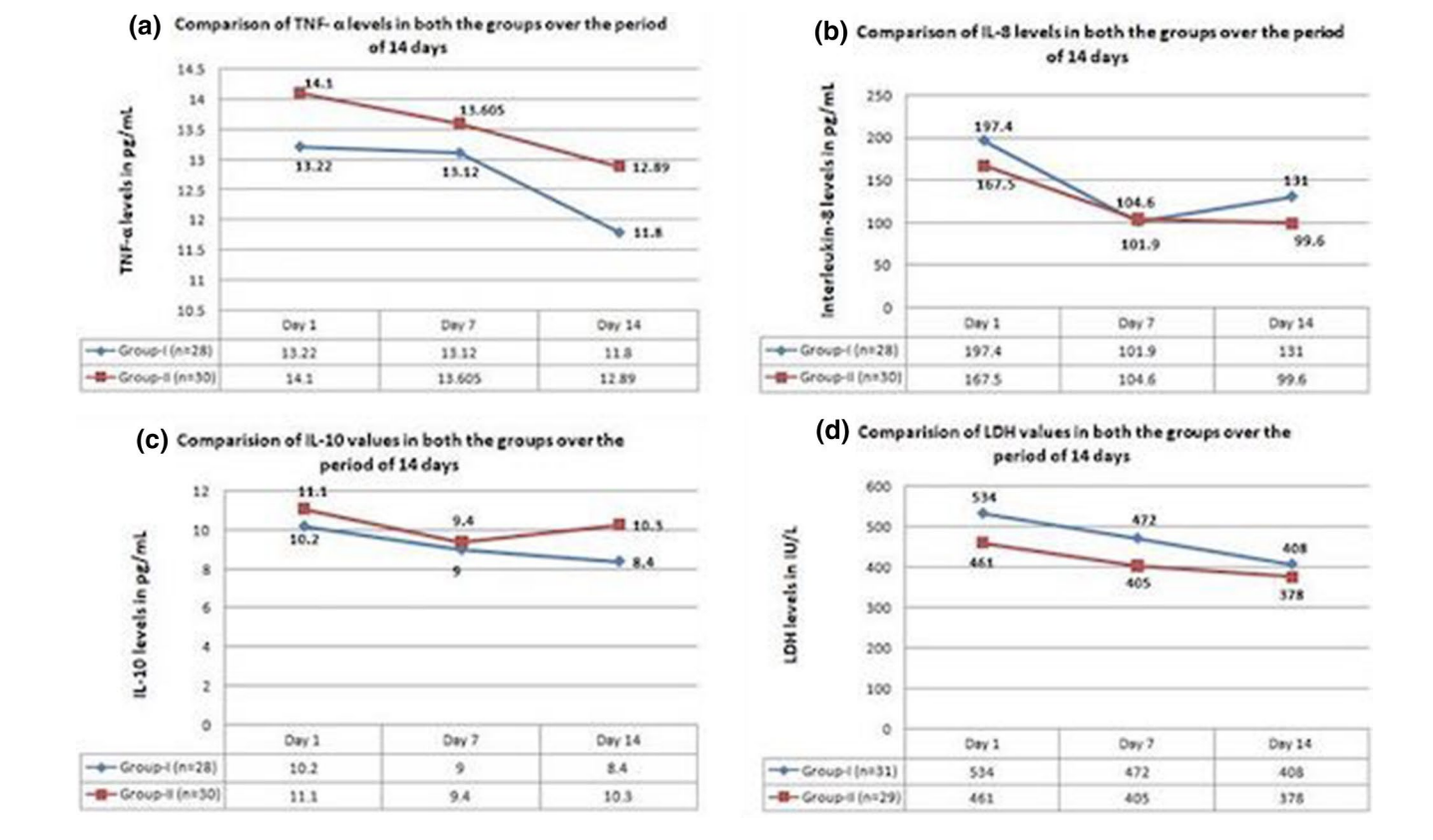
研究结果显示总共有86名患者被随机分配到治疗组与安慰剂组。胰腺炎的人口统计学特征和严重程度具有可比性。两组之间的脓毒症并发症没有显着差异(59% VS 64%;p = 0.59)。白细胞和中性粒细胞总数在前7天显着减少(p = 0.01)。其他炎症标志物未见显着差异。LOH 显着降低(10 VS 7;p = 0.02)。非脓毒症发病率(41% VS 62.2%;p = 0.06)和 ICU 住院时间(3 VS 2;p = 0.06)均有明显改善。
本项研究证实合生元并未显着降低中重度和重度急性胰腺炎患者的脓毒症并发症;但是,它们显着降低了患者的LOH。
原始出处:
Gorrepati Rohith. et al. Effect of Synbiotics in Reducing the Systemic Inflammatory Response and Septic Complications in Moderately Severe and Severe Acute Pancreatitis: A Prospective Parallel-Arm Double-Blind Randomized TrialGorrepati Rohith. Digestive Diseases and Sciences.2022.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














#Dis#
59
#全身炎症反应#
51
#并发#
67
#脓毒性#
51
#炎症反应#
0
#合生元#
35
#全身炎症#
43