Dig Dis Sci: 急性胰腺炎深静脉血栓形成与高死亡率相关
2022-07-31 xuyihan MedSci原创
急性胰腺炎是多种病因导致胰酶在胰腺内被激活后引起胰腺组织自身消化、水肿、出血甚至坏死的炎症反应。
急性胰腺炎 (AP) 是全球最常见因为胃肠道住院的原因之一。AP是一种早期出现细胞因子风暴的全身性疾病,后期会出现各种局部和感染性并发症。许多急性坏死性胰腺炎(ANP)患者需要延长住院时间甚至延长ICU治疗时间,这会增加发生血栓并发症的风险。由于预防性抗凝可导致各种延迟干预或增加出血和推迟的风险,而不使用抗凝药物则会增加四肢血栓的风险(eDVT),急性胰腺炎入院患者的 eDVT 风险尚未得到很好的探究。因此,研究人员进行了一项前瞻性研究,以确定AP发病率和与eDVT发展相关的可能风险因素。
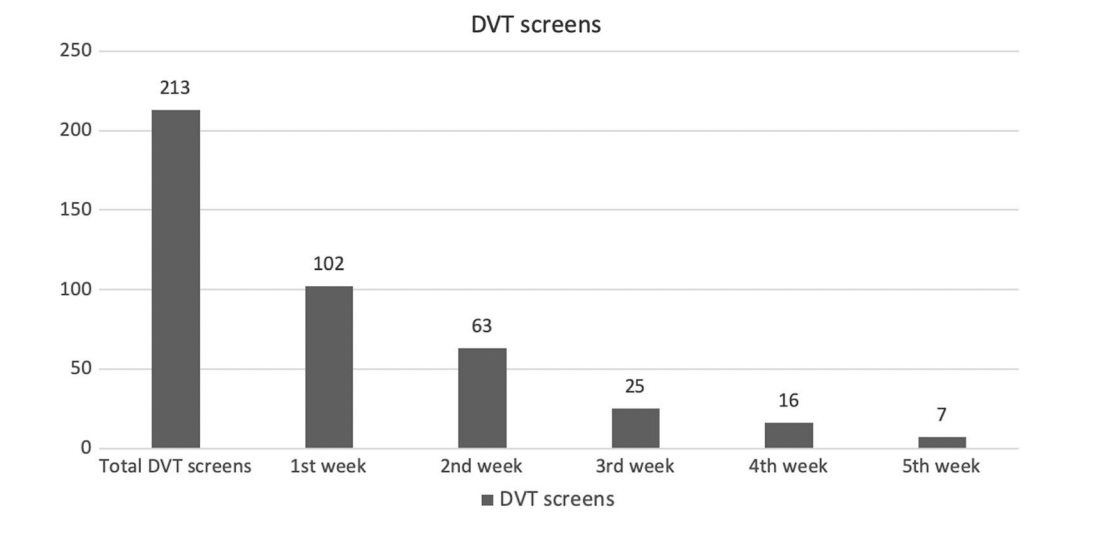
研究人员前瞻性地招募了入院时存在急性胰腺炎的患者,并在入院期间每周进行一次 eDVT 筛查。血栓相关的评分如Well评分和 Padua评分也是每周计算一次。同时靠基于腹部增强 CT 扫描的 eDVT记录了静脉血栓形成的发生率,并使用多变量分析确定了危险因素。使用 Pearson 相关性计算 Well 评分、Padua 评分和 DVT 发展之间的相关性。
研究结果显示在入组的102名急性胰腺炎患者中,73.5%的患者患有坏死性胰腺炎。共有46名患者(45.1%)发生血栓形成:43名患者出现内脏静脉血栓形成;5名患者出现eDVT;1例出现肺栓塞。eDVT患者的BISAP评分较高(2.6 ± 0.9 vs 1.7 ± 0.8;p = 0.039)、机械通气需求(60% vs 8.2%;p = 0.008)和死亡率(60% vs 12.4%;p = 0.022)也较高。Well评分≥2分对 eDVT 预测的敏感性和特异性分别为 80% 和 96.9%,与 Pauda 评分相比,它与eDVT 发展的相关性更好。
本项研究证实在需要入院治疗的急性胰腺炎患者中,DVT的发生率为5%。它与更高的疾病严重程度和死亡率有关。Well 评分可用于预测常规临床实践中eDVT 的发展。
原始出处:
Terence Susngi. et al. Deep Venous Thrombosis in Acute Pancreatitis Is Associated with High Mortality: A Prospective Study. Digestive Diseases and Sciences.2022.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














#Dis#
47
#静脉#
44
#静脉血#
40
#静脉血栓形成#
57