ASCO2017:索拉非尼在晚期肝细胞癌患者中的多中心II期研究
2017-05-20 豆芽菜 艾兰博曼医学网
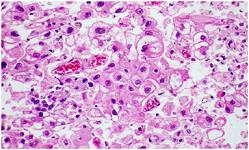
在早期剂量递增研究中,索拉非尼是一种新的口服多激酶抑制剂,在0.2g bid和0.3g bid剂量水平下对治疗不同类型实体瘤包括HCC均显示出抗肿瘤活性和良好耐受性。 这项前瞻性研究旨在评估索拉非尼在晚期HCC患者中的安全性和有效性。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#细胞癌#
40
#ASC#
39
#多中心#
27
#肝细胞#
32
#晚期肝细胞癌#
33
认真学习,不断进步,把经验分享给同好。点赞了!
61
学习并分享!!
41
学习了,再简短点更好
48
学习了,谢谢分享
60
感谢分享一下!!
47