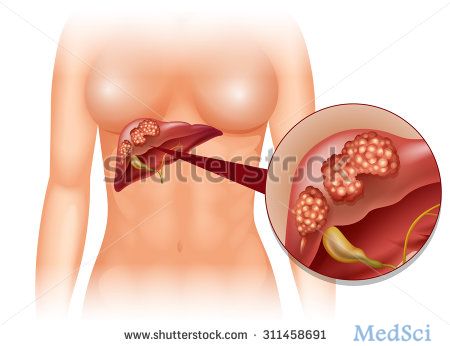
JAMA SURGERY:肝切除术后残余肝组织缺血与肝细胞癌早期复发及不良预后有关
2017-05-06 MedSci MedSci原创
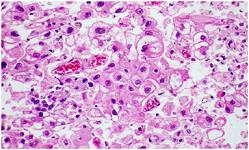
肝切除术后残余肝可能会出现血供不足,尤其是进行非解剖性切除以及存在血管损伤的残余肝,血供不足的情况更为严重。JAMA SURGERY近期报道了一篇文章,评估残余肝缺血(RLI)对于肝细胞癌患者肝切除术后长期生存及死亡率的影响。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#GER#
27
#切除术#
35
#肝组织#
41
#早期复发#
28
#surgery#
42
#肝切除#
42
#肝细胞#
23
#细胞癌#
22
学习
64
厉害厉害学习理论
74