陆国平:选择更为适合中国人群的降脂策略——《中国成人血脂异常防治指南(2016年修订版)》要点解读
2016-11-29 陆国平 门诊新视野微信号
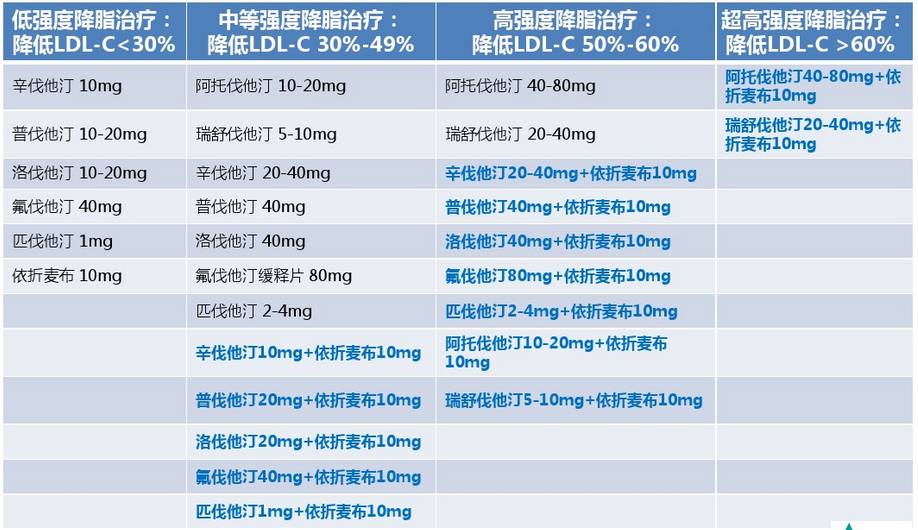
《中国成人血脂异常防治指南(2016年修订版)》(以下简称指南)已于2016年10月24日发布,该版指南距上版已九年有余,自修订起便受到持续关注。新版指南在2007年版《中国成人血脂异常防治指南》的基础上更新,对LDL-C靶目标值、危险分层标准、干预靶目标等方面均作了强调或改变。在指南修订的过程中专家组有哪些思维的碰撞?针对核心问题讨论时又擦出了怎样的火花?《门诊》特别邀请新版指南修订委员会专

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#防治指南#
33
#血脂异常#
34
很好,不错的指南资料,值得拥有值得收藏,值得探究。给自己学习探究提供方便。点个赞!
54
学习了,努力完成目标
49
中国应该有自己的标准
57
非常好,学习了
59
好资料,大家学习下
0
讲的真好,学习了
24
这个很干货
25
学习了,血脂高是很多慢病的危险因素。而不同种族应有不同对策才是。
29