吸烟会导致术后切口深部组织感染?植入物翻修?不是危言耸听!
2016-05-23 译者:龙岩 SIFIC官微
入院时医生都会询问患者吸烟史,手术医生及麻醉医生在术前无一例外地会劝患者术前戒烟,他们一般会告诉患者吸烟会导致术后诸多并发症,如升高血压、诱发心绞痛、支气管哮喘、手术切口感染等,但是相关的循证依据并不多,本文为一个大数据研究,为大家提供了吸烟会引起术后切口深部组织感染和植入物翻修的理论依据。
入院时医生都会询问患者吸烟史,手术医生及麻醉医生在术前无一例外地会劝患者术前戒烟,他们一般会告诉患者吸烟会导致术后诸多并发症,如升高血压、诱发心绞痛、支气管哮喘、手术切口感染等,但是相关的循证依据并不多,本文为一个大数据研究,为大家提供了吸烟会引起术后切口深部组织感染和植入物翻修的理论依据。

正处于吸烟状态会导致全髋关节或膝关节置换术后高植入物翻修率及切口深部组织感染率:一项前瞻性队列研究
背景:
吸烟是引起术后不良结果的危险因素。本文旨在比较当时正处于吸烟状态的患者和非吸烟的患者进行全髋关节置换术(THA)或全膝关节置换术(TKA)后并发症的发生率。
方法:
本项研究的对象为2010–2013年在梅奥诊所行全髋关节置换术(THA)或全膝关节置换术(TKA)的所有患者。这些患者包括吸烟、曾经吸烟及非吸烟者。吸烟者又分为吸卷烟、吸雪茄烟和使用烟管的吸烟者。应用Cox比例风险回归分析、风险比和95%可信区间(CI)评估吸烟与全髋关节置换术(THA)或全膝关节置换术(TKA)术后并发症之间的关系。
结果:
吸烟者7926例(95%),非吸烟者446例(5%),其中565(7%)是当时正处于吸烟状态的患者。吸烟者大多数为男性(p < 0.001),且肥胖者更少(p≤0.008),≥60岁,查尔森得分> 0或全膝关节置换术(TKA)而非全髋关节置换术(THA)(p值均 < 0.001)。切口深部组织感染的风险比(2.37;95%可信区间1.19,4.72;p = 0.01)及植入物翻修风险比(1.78;95%可信区间1.01,3.13;p = 0.04),吸烟者高于非吸烟者。人工关节周围骨折或切口浅表感染没有显著差异。
结论:
研究表明,在原发的全髋(THA)或全膝关节置换术(TKA)术后,正处于吸烟状态的患者发生切口深部组织感染和植入物翻修的风险较高。未来的研究应关注择期手术如全髋和全膝关节置换手术前戒烟的最佳时间,以改善关节成形术术后短期和长期的预后。
表1 按是否吸烟分组,全髋关节置换术或全膝关节置换术患者的特征比较
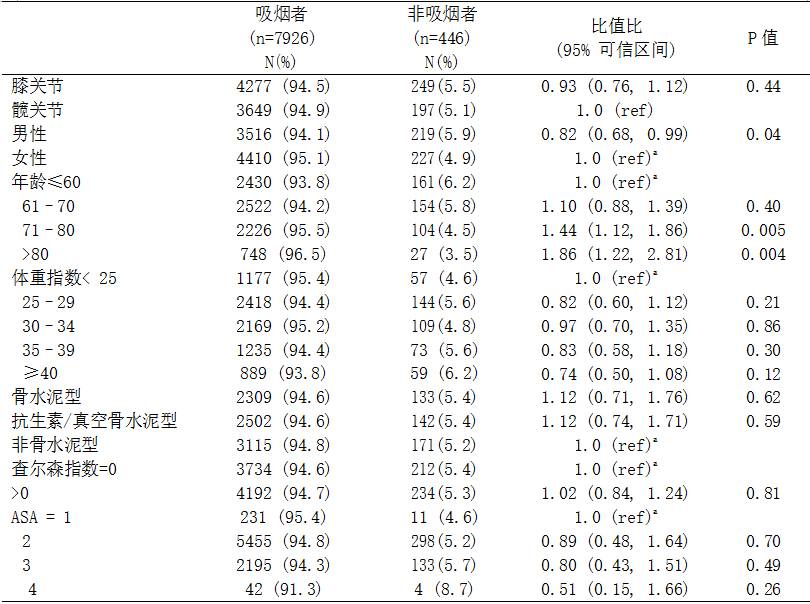
ASA:美国麻醉医师协会, BMI:体重指数, ref:参考类别, SD:标准差
a已对参与组进行了校正(TKA vs. THA)
表2 按是否正在吸烟分组,全髋关节置换术或全膝关节置换术患者的特征
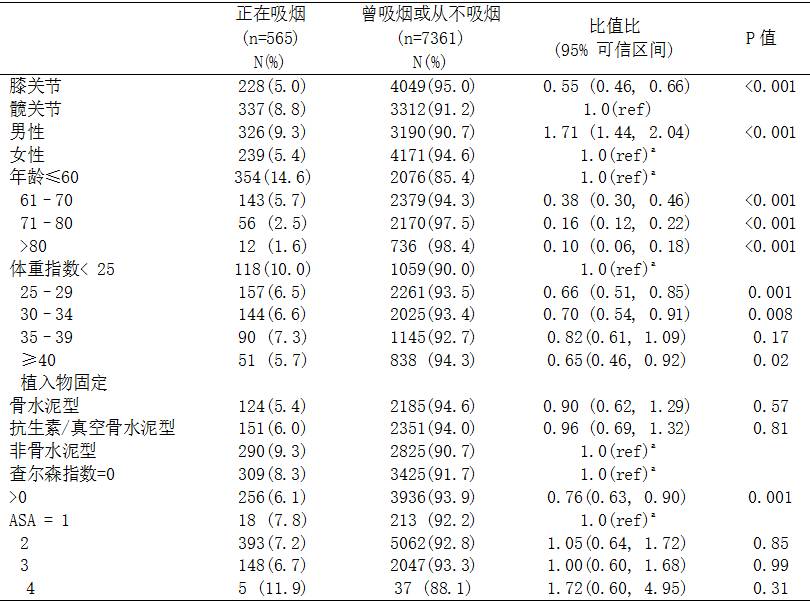
ASA 美国麻醉医师协会, BMI 体重指数, ref 参考类别, SD 标准偏差
a已对参与组进行了校正(TKA vs. THA)
表3 按是否是正在吸烟的患者进行校正的关节类型和每种并发症多变量校正的风险
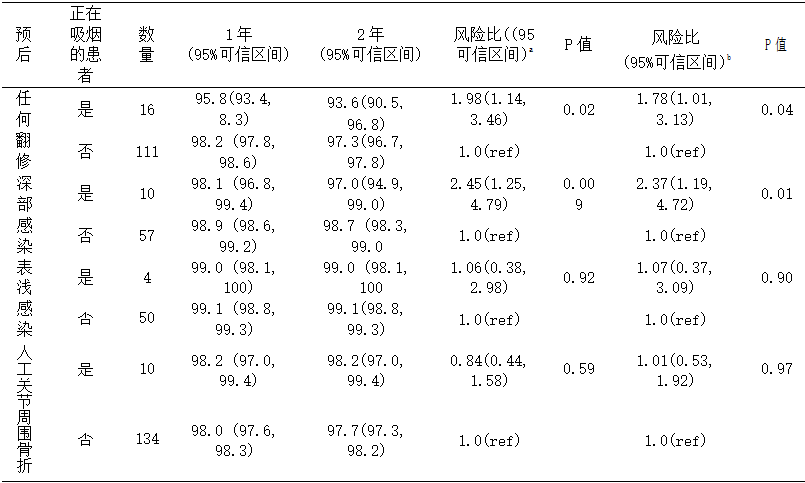
a膝关节Cox模型 (与髋关节对比);b校正后的膝关节Cox模型 (与髋关节对比),男性 (与女性对比),手术后的年龄 (每年),风险比和p值均有显著意义。
原始出处:
Jasvinder A. Singh, Cathy Schleck, W. Scott Harmsen, AdamK. Jacob, David O. Warner and David G. Lewallen.Current tobacco use is associated with higher rates of implant revision and deep infection after total hip or knee arthroplasty: a prospective cohort study. Singh et al. BMC Medicine (2015) 13:283.
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







文章不错,值得拜读
41
#植入物#
31
#植入#
34