LANCET:经皮硝酸甘油可有效控制急性卒中发作后高血压
2015-02-18 梁怀彬 译 MedSci原创
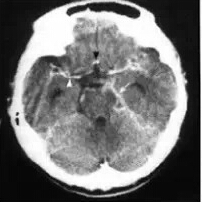
卒中后高血压可能导致不良的转归,卒中后早期血压是否应该降低、是应该继续服用卒中前就已在服用的降压药物还是短暂撤除降压药这些问题一直争论不休,研究者为此开展实验评估中风后使用降压药对卒中后转归影响。在这项多中心的实验中,研究者将入院的急性缺血性脑卒中和出血性脑卒中的高血压患者(收缩压140-220mm Hg)一部分患者采用经皮硝酸甘油渗透连续7天(5mg每天)。均开始于中风发作后48h内。对照组不给
卒中后高血压可能导致不良的转归,卒中后早期血压是否应该降低、是应该继续服用卒中前就已在服用的降压药物还是短暂撤除降压药这些问题一直争论不休,研究者为此开展实验评估中风后使用降压药对卒中后转归影响。

从2010年7月20日到2013年10月14日,研究者收集了4011名卒中患者,基线平均血压是167±19mmHg/90±13 mmHg(卒中发作后中位时间26h[16–37]),甘油三酯组的2000名患者和对照组的2011名患者相比第一天血压显著下降(差值−7·0 [95% CI −8·5 to −5·6] mm Hg/–3·5 [–4·4 to −2·6] mm Hg; both p<0·0001),1503名持续使用降压药的患者和1044名暂停降压药患者相比在第七天血压也呈现明显下降(差值−9·5 [95% CI −11·8 to −7·2] mm Hg/–5·0 [–6·4 to −3·7] mm Hg; both p<0·0001)。第90天后的功能转归指标(调整一般OR值后)各组没有明显差别:不良转归上硝酸甘油组相比未使用硝酸甘油组优势比OR为1.01(95% CI 0·91–1·13; p=0·83),持续服用降压药组相比暂时中断降压药组优势比OR为1.05(0·90–1·22; p=0·55)。
急性中风合并高血压的患者,经皮硝酸甘油能有效降低血压,安全性良好,但是不能改善功能转归。尚无充分证据支持卒中前降压药物在急性卒中后的前几日有持续继续使用的必要。
原始来源:
The ENOS Trial Investigators.Efficacy of nitric oxide, with or without continuing antihypertensive treatment, for management of high blood pressure in acute stroke (ENOS): a partial-factorial randomised controlled trial.Lancet. 2014 Oct 21. pii: S0140-6736(14)61121-1. doi: 10.1016/S0140-6736(14)61121-1. [Epub ahead of print]
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#Lancet#
37
不错的文章,学习了
77
#急性卒中#
43
#硝酸甘油#
35
经皮?
97
明白了
77
?
97
家中老人必看
124
好厉害。
70