盘点:冠心病2016年相关指南更新及共识(二)
2016-09-27 MedSci MedSci原创
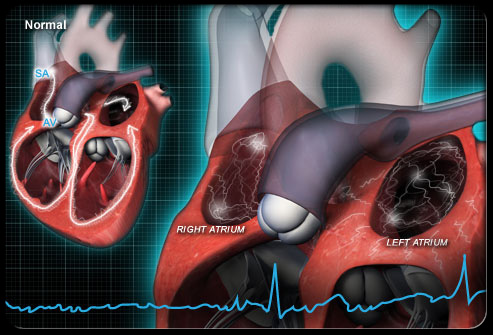
冠心病是全球常见病、多发病,严重危害人类健康和生存质量。尽管近年来心血管疾病的诊疗方法已取得突飞猛进的发展,但其死亡率仍占全世界总疾病死亡率的30%,远远超过癌症等其他疾病,预计到2030年由心血管疾病造成的花费将达到10440亿美元。这里小M整理了今年以来冠心病方面的指南与共识与大家分享,与大家分享。(冠心病2016年相关指南更新及共识(一))【1】2016 高龄老年冠心病诊治中国专家共识稳
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#指南更新#
37
学习了,多谢分享!
55
学习了,多谢分享!
62
学习了,多谢分享!
74
学习了,多谢分享!
57
学习了,多谢分享!
68
赞一个!!
24
赞一个!!!!!!
29
很好!!!!!!
27
很不错!
27