Neurol Neuroimmunol Neuroinflamm:组织谷氨酰胺酶表达与多发性硬化的进展有关
2021-06-23 MedSci原创 MedSci原创
PBMCs来源的TG2 mRNA水平与多发性硬化疾病进展的临床和放射学测量相关,因此有望作为多发性硬化特别是PP多发性硬化患者疾病进展的生物标志物。
多发性硬化症(MS)是中枢神经系统的一种慢性炎症性神经退行性疾病。它是导致年轻人永久残疾的最常见的神经疾病。严重程度和临床病程因患者而异,很大程度上是不可预测的。如今,临床上使用的生物标志物很少,大多数检测从临床孤立综合征到MS的转化或对治疗的反应此外,他们大多依赖脑脊液采集,这是一个有创的过程。神经丝轻链蛋白(NfL)正在成为MS中最有前途的生物标志物。然而,NfL与疾病进展的相关性不太准确。因此,对预测多发性硬化症进展的血源性生物标志物的需求尚未得到满足。
多发性硬化症(MS)的临床过程是可变的,很大程度上不可预测,迫切需要标志物来监测疾病的活动和进展。最近的证据显示,组织转谷氨酰胺酶(TG2)在患者来源的单核细胞中发生改变。TG2可以作为宫颈发育不良的生物标志物,此外,抗TG2抗体被用作腹腔疾病诊断的血清学标志物。然而,TG2作为血液源性生物标志物在多发性硬化中的潜在应用尚未得到研究。
最近Neurol Neuroimmunol Neuroinflamm杂志发表文章,假设血液细胞来源的TG2信使RNA (mRNA)可能被用作MS患者的生物标志物。该研究评估MS患者外周血单核细胞(PBMC)来源的TG2是否发生改变,以及TG2信使RNA (mRNA)是否与疾病活动和/或进展相关。
在外周血单核细胞(PBMCs)中,从151个健康对照和161例患者中,测量了TG2 mRNA,与疾病活动的临床和MRI参数(年化复发率、高含量的病变、T2病灶体积)和疾病进展(扩展残疾状态量表[EDSS],标准化脑体积和T1低信号病灶体积)相关。

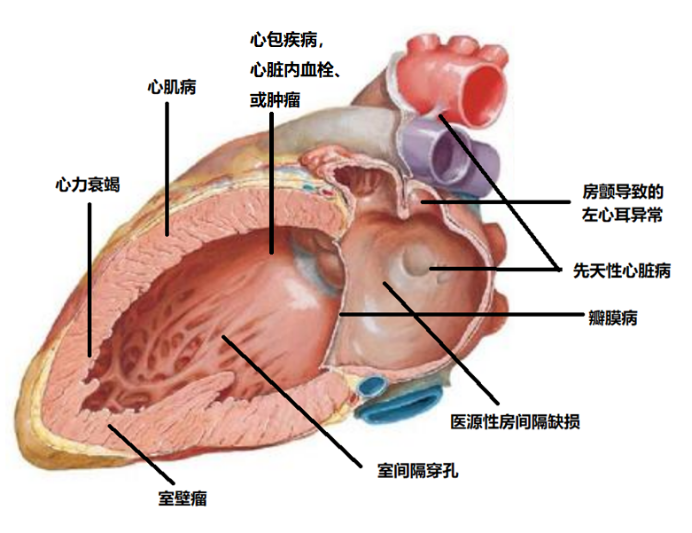
TG2与MS患者和MS各亚型疾病进展指标的相关性。PBMCs来源的TG2 mRNA水平与(A)扩展残疾状态量表(EDSS)的相关性。(B) 2年随访后EDSS相对变化;(C)标准化脑体积(NBV);(D)标准化灰质体积(NGMV), (E)标准化白质体积(NWMV)。PBMCs来源的TG2 mRNA水平与(G) EDSS; (H) NBV;(I)NGMV;(J) NWMV;(K) T1病灶体积(T1LV) (LogT1LV) 的相关性。对性别和年龄进行线性回归分析。
PBMC来源的TG2 mRNA水平与疾病进展显著相关(总MS患者组的2年随访EDSS恶化、以及基线标准化脑体积、标准化灰白质体积)。其中,在复发-缓解MS患者中,TG2表达与2年随访EDSS评分的恶化显著相关。在原发性进展性(PP) MS患者中,TG2 mRNA水平与EDSS、标准化脑体积、标准化灰白质体积显著相关。此外,在基线时,在PP MS患者中,TG2 mRNA与T1低信号病变体积相关。
到目前为止,许多针对多发性硬化症疾病活动和进展的候选生物标志物都是在脑脊液中测量的,而脑脊液只能通过侵入性程序收集,因此脑脊液来源的生物标志物与血液来源的标志物相比对患者不太方便,特别是在需要重复测量的情况下。目前迫切需要一种生物标志物来预测和监测疾病的长期进展,并反映进展中患者的轴突损伤。迄今为止,NfL似乎最有希望作为MS疾病活动的标记物,对DMDs的反应也在血清样本中得到验证。尽管最近的一些文章也表明与多发性硬化症的疾病进展有关,这还有待证实。此外,血清胶质纤维酸性蛋白水平已被提出作为PP MS患者疾病严重程度的生物标志物,但未发现与MRI参数相关。
总之,该研究中报道的新发现表明,PBMCs来源的TG2 mRNA水平与多发性硬化疾病进展的临床和放射学测量相关,因此有望作为多发性硬化特别是PP多发性硬化患者疾病进展的生物标志物。
原文出处
Tissue Transglutaminase Expression Associates With Progression of Multiple Sclerosis, Claudia Sestito, Cyra E. Leurs, Martijn D. Steenwijk, John J.P. Brevé, Jos W.R. Twisk, Micha M.M. Wilhelmus, Benjamin Drukarch, Charlotte E. Teunissen, Anne-Marie van Dam, Joep Killestein, Neurol Neuroimmunol Neuroinflamm Jul 2021, 8 (4) e998; DOI: 10.1212/NXI.0000000000000998
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#LAM#
40
#酶表达#
31
#Neurol#
25
#多发性#
36
#NFL#
36
好
54