Nat Med:过量鞘脂合成会引起儿童肌萎缩侧索硬化
2021-06-01 xiaozeng MedSci原创
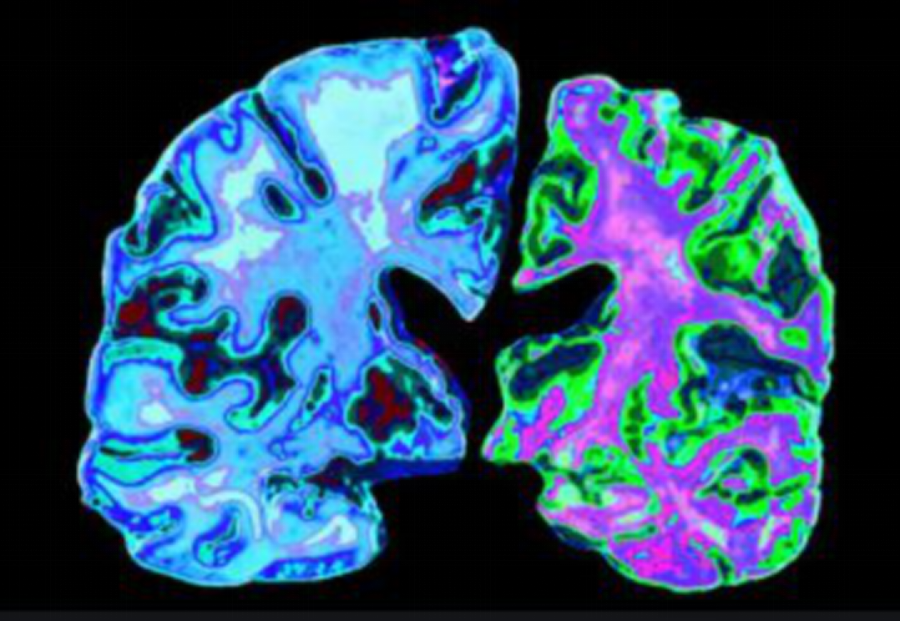
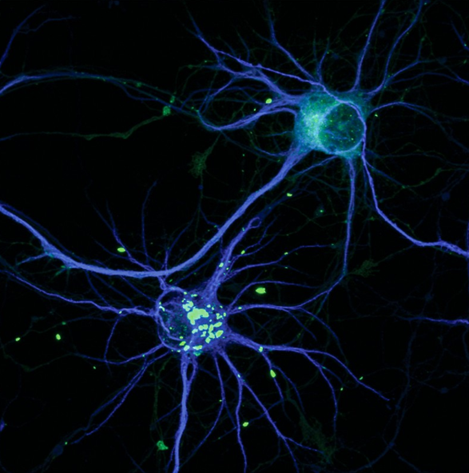
肌萎缩侧索硬化(ALS)是一种散发性或遗传性的进行性神经退行性疾病,ALS患者的发病年龄、运动神经元变性模式和疾病进展差异很大。
肌萎缩侧索硬化(ALS)是一种散发性或遗传性的进行性神经退行性疾病,ALS患者的发病年龄、运动神经元变性模式和疾病进展差异很大。
除了通常在55至75岁之间出现的更常见的散发性ALS之外,具有单基因遗传性致病突变是越来越多的家族性和早发性ALS病例的一大基础特征。其可为疾病提供独特的机制和病理生理学见解,并可指导合理的治疗策略的制定。
虽然ALS的发病机制涉及多种细胞过程,但迄今为止尚未发现单基因代谢紊乱与ALS之间的相关性。
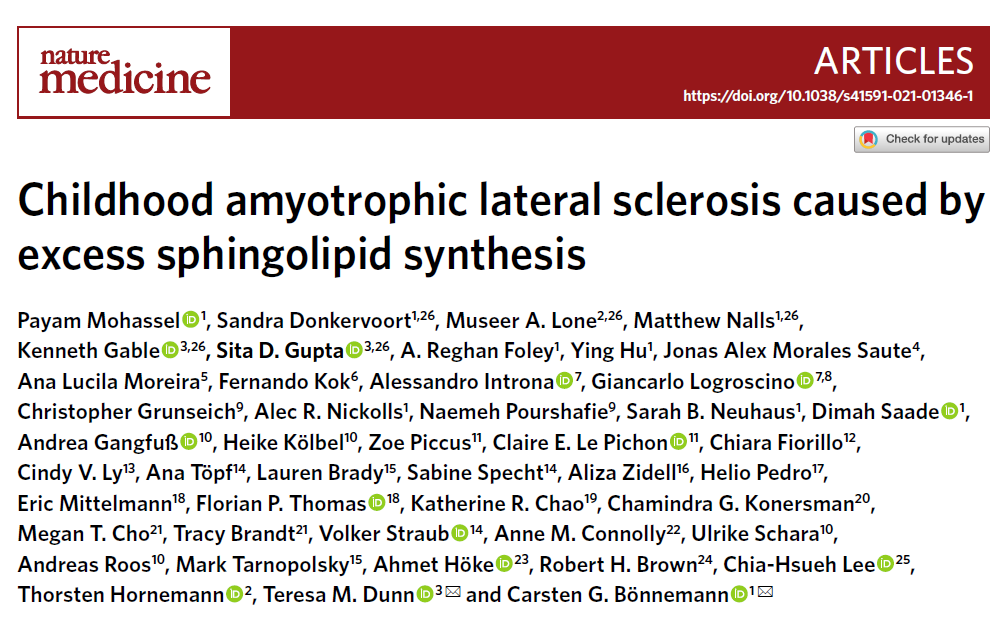
在该研究中,研究人员发现,能够导致无限制的鞘脂合成的SPTLC1突变体,会诱发单基因突变型ALS。研究人员在七个表现为儿童期ALS的家系中确定了四种特定的、显性的SPTLC1突变体。
儿童期ALS患者的SPTLC1突变信息
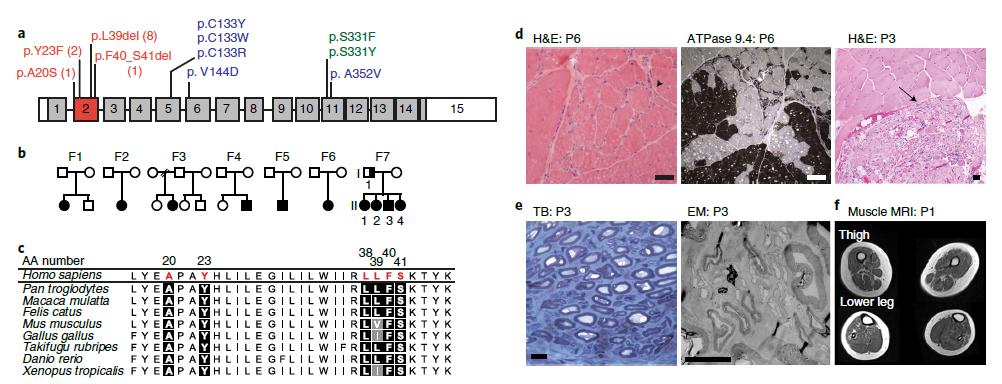
这些突变破坏了ORMDL蛋白对SPT(丝氨酸棕榈酰转移酶)的正常稳态调节,导致SPT活性不受调节以及经典SPT产物水平的升高。值得注意的是,通过比对SPTLC1突变体的形成,研究人员发现,SPT改变的氨基酸从丝氨酸转变为丙氨酸,会导致脱氧鞘脂水平的升高,并表现为遗传性感觉和自主神经病变的替代表型。
研究人员通过小干扰RNA选择性靶向SPTLC1的ALS等位基因并进行降解,能够保持正常等位基因的完整,并使体外鞘脂的水平正常化。而原发性代谢紊乱在ALS中的作用仍然未知。
ORMDL蛋白介导的SPT稳态调节
综上,该研究结果揭示,过量的鞘脂生物合成或与运动神经元相关疾病的发病机制相关。
原始出处:
Mohassel, P., Donkervoort, S., Lone, M.A. et al. Childhood amyotrophic lateral sclerosis caused by excess sphingolipid synthesis. Nat Med (31 May 2021).
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#萎缩#
34
#Nat#
31
#肌萎缩#
36
#肌萎缩侧索硬化#
44
#Med#
35
已读,真是受益匪浅呀。
62
学习了
50