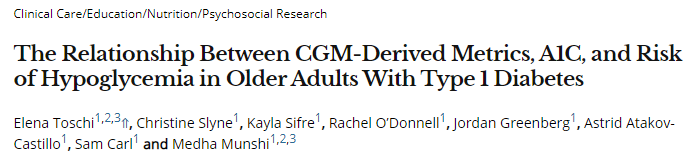
Diabetes Care:CGM衍生指标、A1C与1型糖尿病老年患者低血糖风险的关系
2020-09-29 MedSci原创 MedSci原创
连续血糖监测(CGM)目前普遍应用于1型糖尿病(T1D)的管理。CGM衍生的变异系数(CV)测量血糖变异性,血糖管理指标(GMI)测量平均血糖(以前称为估计A1C)。然而,它们与实验室测量的A1C和T
连续血糖监测(CGM)目前普遍应用于1型糖尿病(T1D)的管理。CGM衍生的变异系数(CV)测量血糖变异性,血糖管理指标(GMI)测量平均血糖(以前称为估计A1C)。然而,它们与实验室测量的A1C和T1D老年人低血糖风险的关系尚未清楚。一项单中心研究纳入T1D的老年人(年龄≥65岁),佩戴CGM装置14天,计算了CV(%)和GMI,并收集了A1C和临床及人口学资料,研究结果已在线发表于Diabetes Care。
结果,研究人员共评估了130名老年人(年龄71±5岁),其中55%为女性,97%为白人,糖尿病持续时间为39±17年,A1C为7.3±0.6%(56±15mmol/mol)。参与者按高CV(>36%;n = 77)和低CV(≤36%;n = 53)分层。尽管高CV和低CV组之间的A1C水平没有差异(7.3%[56 mmol/mol]vs.7.3%[53 mmol/mol],P = 0.4),但与低CV组相比,高CV组在低血糖状态下花费的时间更多(<70 mg/dL和≤54 mg/dL)(中位数31 vs.84 min/天,P <0.0001;8 vs.46 min/天,P <0.001)。46%的队列中,A1C和GMI的绝对差异≥0.5%。当A1C高于GMI≥0.5%时,观察到较高的低血糖持续时间(P = 0.02)。
综上所述,该研究结果表明,在患有T1D的老年人中,与单纯的A1C相比,使用CGM衍生的CV和GMI可以更好地识别低血糖高风险的个体。这些测量方法应与A1C相结合,以便更好地管理T1D老年人的糖尿病。
原始出处:
Elena Toschi, Christine Slyne, et al., The Relationship Between CGM-Derived Metrics, A1C, and Risk of Hypoglycemia in Older Adults With Type 1 Diabetes. Diabetes Care 2020 Oct; 43(10): 2349-2354. https://doi.org/10.2337/dc20-0016.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言




.jpg)






#Diabetes#
34
#DIA#
38
#风险的关系#
50
#CGM#
0
😊😊😊😊😊
99
#BET#
33
谢谢MedSci提供最新的资讯
42