J Gastroenterology: 血管性血友病因子抗原与血小板比率(VITRO)评分可预测肝硬化患者的肝失代偿和死亡率
2020-05-01 MedSci原创 MedSci原创
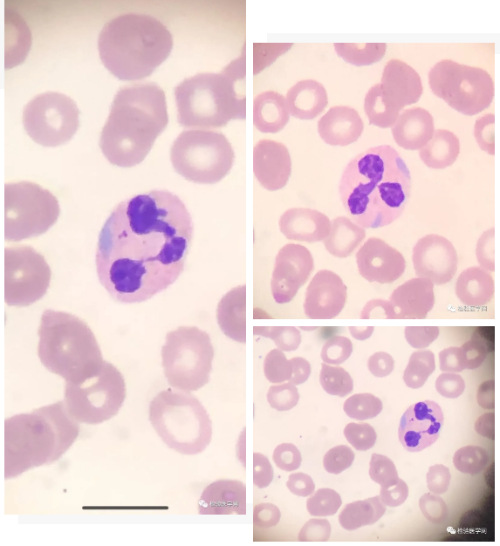
血管性血友病因子与血小板的比例(VITRO)反映了肝硬化患者肝纤维化和门脉高压的严重程度,因此可能具有预后价值。
背景: 血管性血友病因子与血小板的比例(VITRO)反映了肝硬化患者肝纤维化和门脉高压的严重程度,因此可能具有预后价值。
方法: 研究人员招募患有代偿性肝硬化的患者。在研究开始时确定了VITRO,Child–Pugh评分(CPS)和MELD的水平。肝代偿失调定义为静脉曲张破裂出血,腹水或肝性脑病。记录肝移植和死亡。
结果: 本项研究共包括194例肝硬化代偿患者(CPS-A 89%,B 11%;男性56%;中位年龄56岁;静脉曲张50%)。在45个月的中位随访期间,失代偿发生35例(18%),14例(7%)患者出现死亡。在n= 88(45%)VITRO≥2.5的患者中,肝失代偿的风险显着增加(p<0.001)。VITRO≥2.5的患者发生失代偿的可能性更高,在1年时为9%(95%CI 3-16%),2年时为18%(95%CI 10–27%),而VITRO <2.5的患者则为4%(95%CI 0–8%)。VITRO≥2.5的患者,估计的1年/ 2年生存率分别为98%(95%CI 95–100%)和94%(95%CI 88–99%),而VITRO <2.5的患者生存率为100%(p <0.001)。调整年龄,白蛋白和MELD后,VITRO≥2.5仍可作为无肝移植患者死亡率的重要预测指标(HR 1.38,CI 1.09–1.76;p = 0.007)。根除丙型肝炎后代偿期肝硬化且VITRO> 2.1的患者失代偿风险仍显着增加(p = 0.033)。
结论: VITRO是评估有价值的肝硬化患者(包括根除丙型肝炎后的环境)失代偿和死亡风险的预后工具。
原始出处:
Rémy Schwarzer. Et al. The von Willebrand Factor antigen to platelet ratio (VITRO) score predicts hepatic decompensation and mortality in cirrhosis. J Gastroenterology.2020.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#Gastroenterol#
37
#血管性#
37
#AST#
36
#血友病因子#
51
#GAS#
30
#Gastroenterology#
30
#抗原#
37
谢谢!最新的信息读起来就是收获大
56