JBMR:唑来磷酸对脊髓损伤后骨质流失的耐受性和延迟治疗的效果
2021-10-26 从医路漫漫 MedSci原创
急性脊髓损伤(SCI)后单次输注唑来膦酸(ZOL)可减轻髋部(股骨近端)和膝关节(股骨远端和胫骨近端)的骨丢失,至少维持6个月。

背景:急性脊髓损伤(SCI)后单次输注唑来膦酸(ZOL)可减轻髋部(股骨近端)和膝关节(股骨远端和胫骨近端)的骨丢失,至少维持6个月。这项研究的目的是检查ZOL在两年内的作用时间和用药频率对SCI的影响。
方法:在这项双盲、安慰剂对照试验中,我们随机选择了60名急性脊髓损伤患者(受伤天数小于120天),接受ZOL 5mg输注(n=30)或安慰剂(n=30)治疗。12个月后,各组再次随机接受ZOL或安慰剂治疗,结果是分析第二年的四个治疗组:(I)ZOL治疗两年;(II)第一年ZOL治疗,第二年安慰剂治疗;(III)第一年安慰剂治疗,第二年ZOL治疗;(Iv)安慰剂两年。
结果:我们的主要结果是12个月时的骨丢失量。与安慰剂相比,单次注射ZOL减轻了股骨近端的骨丢失,与基线相比,ZOL的中位数变化是-1.7%到-2.2%,而安慰剂是-11.3%到-12.8%(p<0.001)。类似的,ZOL组股骨远端和胫骨近端的变化为4.7%到9.6%,而安慰剂组为8.9%到23.0%(p≤0.042)。24个月后,仅在股骨近端有显著差异(ZOL组为3.2%至6.0%,安慰剂组为16.8%至21.8%;p≤0.018)。虽然在统计学上没有显著意义,但骨密度下降的中位数表明,与单次基线输注ZOL相比,每年两次输注,以及与安慰剂2年相比,基线后12个月单次输注ZOL都有一定的益处。因此,有必要在12个月至24个月的治疗窗口进行进一步研究。没有观察到与药物治疗相关的不良事件。
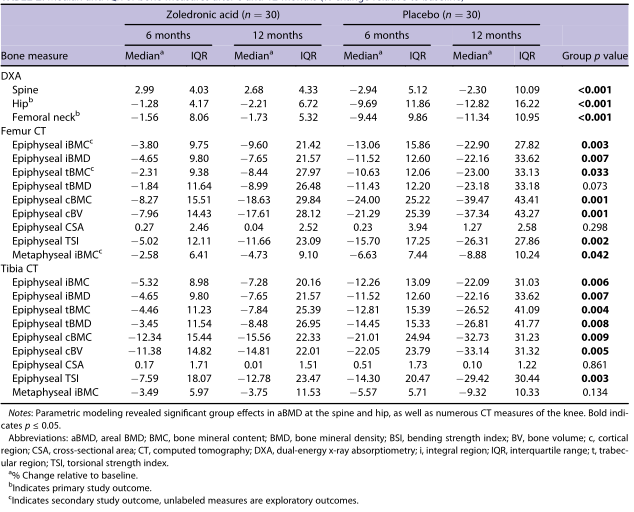
表1 6个月和12个月后骨测量的中位数和IQR(相对于基线的百分比变化)
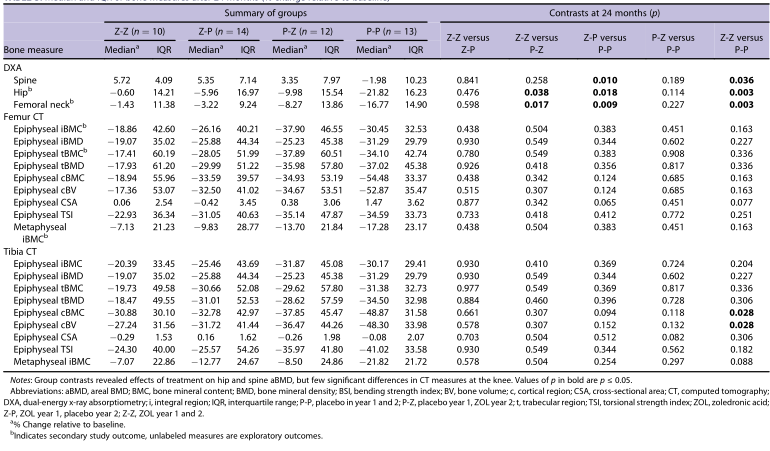
表2 24个月后骨测量的中位数和IQR(相对于基线的百分比变化)

图 所选骨骼测量在研究期间的变化。数据表示为相对于基线变化的中位数和IQR百分比。在第一年,参数建模显示服用ZOL的个体与服用安慰剂的个体之间存在显著差异(*p<0.05)。第二年后,小组对比显示,与全程服用安慰剂的人相比,在第一年服用ZOL的人在脊柱和髋部的骨密度继续表现出改善(†p<0.05vs.2年安慰剂组)。然而,第2年时,两组间几乎没有膝关节CT测量有显著差异。缩写:aBMD,面骨密度;CT,CT;FN,股骨颈;IBMC,积分骨矿含量;IQR,四分位数范围;ZOL,唑来膦酸。
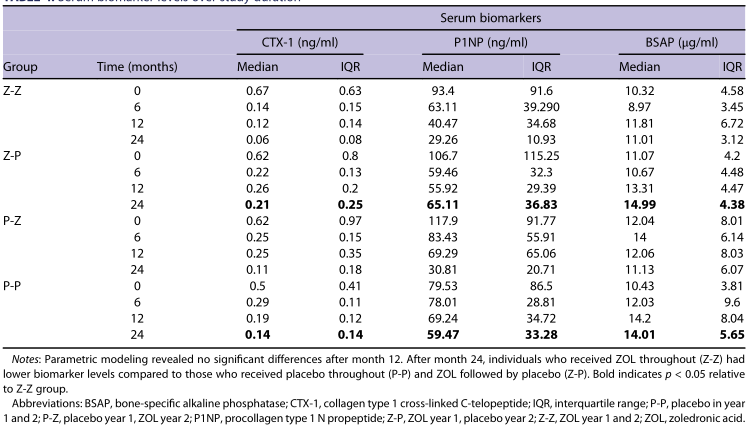
表3 研究期间的血清生物标志物水平
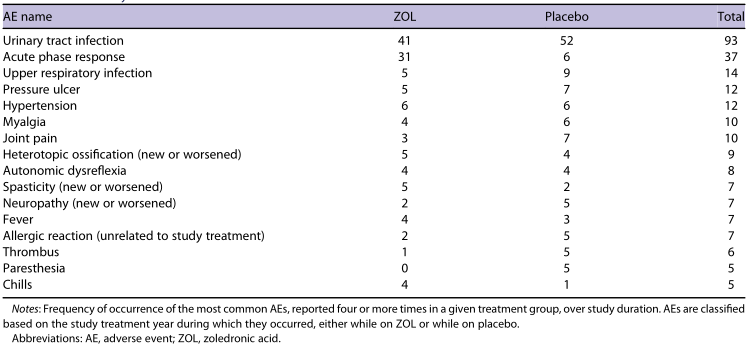
表4 AE总结
结论:综上所述,急性脊髓损伤后输注ZOL 5 mg耐受性良好,可能为预防脊髓损伤后最初几年的骨丢失提供一种有效的治疗方法。
原文出处:
Edwards WB, Haider IT, Simonian N,et al,Durability and delayed treatment effects of zoledronic acid on bone loss after spinal cord injury: a randomized, controlled trial.J Bone Miner Res 2021 Jul 19
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#骨质流失#
38
#损伤#
27
#耐受性#
36
#骨质#
0