Science:少突胶质细胞如何通过血管进入大脑?
2016-02-01 佚名 生物谷
图片来源:medicalxpress.com 来自美国加州大学旧金山分校(UC San Francisco)的科学家近日通过研究发现,产生髓磷脂的细胞可以通过在血管中以“攀爬摆动”的方式迁移到发育中的大脑中,同时研究者还发现了一种特殊机制,即名为寡突细胞(少突胶质细胞)的未成熟细胞如何离开血管从而分化成为成熟的寡突细胞,寡突细胞可以将自身包裹于神经纤维中来加速神经传导,相关研究刊登于国际杂志

图片来源:medicalxpress.com
来自美国加州大学旧金山分校(UC San Francisco)的科学家近日通过研究发现,产生髓磷脂的细胞可以通过在血管中以“攀爬摆动”的方式迁移到发育中的大脑中,同时研究者还发现了一种特殊机制,即名为寡突细胞(少突胶质细胞)的未成熟细胞如何离开血管从而分化成为成熟的寡突细胞,寡突细胞可以将自身包裹于神经纤维中来加速神经传导,相关研究刊登于国际杂志Science上。
研究者Stephen Fancy说道,人类拥有大量和大脑尺寸相当的有髓神经纤维(myelinated nerve fibers),但这些细胞如何迁移到大脑中也是一个困扰科学家们多年的研究课题,本文研究中,研究者就揭示了少突胶质前体细胞(oligodendrocyte precursor cells,OPCs)如何分化成为成熟形式的细胞,此前研究发现,Wnt信号通路可以抑制上述转化过程,直到细胞处于正确位置开始形成髓磷脂,但研究者表示,当其在小鼠机体中锁定为高水平的Wnt信号时,前体细胞就会出现迁移问题,进而开始卡在血管中。
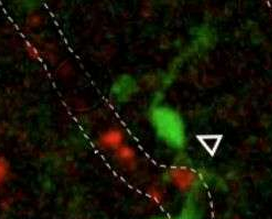
随后研究者对小鼠发育中的大脑中的少突胶质前体细胞进行活体成像分析,结果发现少突胶质前体细胞可以在血管中“慢行”同时还可以伸直其胳膊样的伸长物来在不同血管间跳跃,研究者还在人类大脑中观察到了相同的过程,这就表明,少突胶质前体细胞的确可以在血管中攀爬及来回摆动。当小鼠大脑不能构建血管时,前体细胞的迁移就会停滞,而当Wnt信号通路被阻断后,就会引发前体细胞在遍布大脑的血管中“跌落”,这就意味着Wnt信号可以在迁移过程中维持和血管相关的细胞。
Fancy说道,似乎Wnt信号在协调迁移和分化时间上扮演着双重的角色,首先其可以以未成熟的形式保持住细胞,直到其可以沿着血管进行迁移,随后当细胞达到目的地后Wnt信号就会指导细胞停止“攀爬”并且开始变得成熟。研究者很希望本文研究可以帮助改善诸如多发性硬化症等多种疾病的发生。
当机体免疫系统攻击并且杀灭产生髓磷脂的少突神经胶质细胞时就会引发多发性硬化症,进而阻断神经传输,引发一系列症状,比如视力缺失、机体麻木、肌无力、机体痉挛、情绪摇摆甚至认知能力下降,病人通常会出现周期性复发的过程,而当大脑尝试通过移除被免疫系统破坏的髓磷脂后患者就会恢复过来。
研究者希望通过阐明少突神经胶质细胞如何迁移到髓磷脂损伤的位点,来帮助降低多发性硬化症患者疾病的复发;目前有很多药物可以帮助减少多发性硬化症患者机体中的脱髓鞘作用,但却并没有有效的疗法来帮助进行髓鞘再生;研究者希望后期可以通过更为深入的研究来为改善多发性硬化症患者的新型疗法提供思路和帮助。
原始出处:
Hui-Hsin Tsai,Jianqin Niu1,et al,Oligodendrocyte precursors migrate along vasculature in the developing nervous system,Science,2016
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#少突胶质细胞#
35
#SCIE#
24
#胶质细胞#
30
学习到了
108
文章bu错
110
赞一个
113
看不懂
99
文章不错
109