急性肺血栓栓塞症rt-PA静脉溶栓致严重低血压
2017-10-21 熊长明 肺血管病
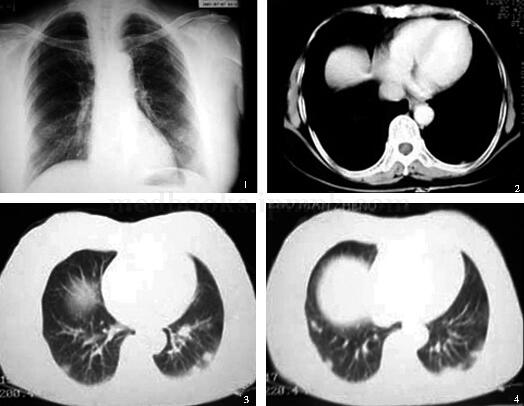
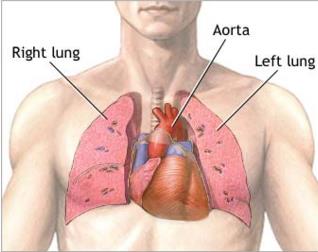
53岁男性,因双下肢外伤1个月,咳嗽,左侧胸痛2天入院。入院诊断:1.急性肺栓塞,2.左下肢深静脉血栓形成。给予重组组织型纤溶酶原激活物(rt-PA)100mg静脉溶栓,但溶栓至1小时10分钟,患者突感头晕,胸闷,面色苍白,查BP 30/0mmHg,HR 40次/分,心电图显示心动过缓,这是为何?
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#栓塞症#
25
#肺血栓#
37
#肺血栓栓塞症#
32
#静脉#
30
#rt-PA#
26
#t-PA#
40
#t-PA静脉溶栓#
32
请问低血压反应的机制是什么?
48
#低血压#
22
溶栓治疗致低血压.学习了.
58