2021 CSBrS实践指南:超声引导下真空辅助乳腺活检
2021-06-07 乳腺外科学会 乳腺外科学会
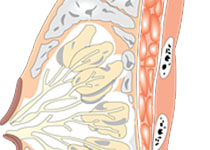
乳房纤维腺瘤是妇女最常见的良性肿瘤,可发生在所有年龄段,常见于15-35岁的女性。
乳房纤维腺瘤是妇女最常见的良性肿瘤,可发生在所有年龄段,常见于15-35岁的女性。
大多数乳腺纤维腺瘤往往是自我限制性生长,通常在几年后稳定下来。临床诊断主要是基于临床触诊和超声检查。诊断主要基于临床触诊和超声检查,而金标准病理检查是诊断的黄金标准。
为了规范乳腺纤维腺瘤的临床诊断和治疗。中华医学会乳腺外科分会(CSBrS)对专家意见进行了文献综述,并确定了文献综述和专家意见,并确定了乳腺纤维腺瘤临床实践指南的关键临床问题。以制定乳腺纤维腺瘤的临床实践指南。
课题组采用建议分级法评估了相关证据,并制定了乳腺纤维腺瘤临床实践指南。
CSBrS实践指南2021,其目的是为为中国的乳腺外科医生提供临床实践指导。
详情参见:2021 CSBrS实践指南:超声引导下真空辅助乳腺活检(需要中文翻译的,请在下方评论哦,超过20个求翻译评论,我们将对此篇进行翻译哦~)
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








求翻译
15
#超声引#
32
#实践指南#
29
求翻译
53
#超声引导#
34
#活检#
28
#乳腺活检#
39
乳房纤维腺瘤是妇女最常见的良性肿瘤,可发生在所有年龄段,值得关注
49
学习了
59